Minimally invasive simple prostatectomy: Robotic-assisted versus laparoscopy. A comparative study
Accepted: February 21, 2022
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
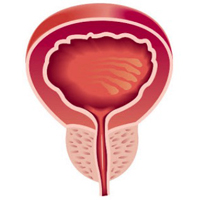
Purpose: Robotic-assisted simple prostatectomy (RASP) is a novel surgical procedure for the management of obstructive symptoms caused by enlarged prostate glands. Before the introduction of minimally invasive techniques, the standard approach was the open simple prostatectomy (OSP). The aim of our study was to compare intraoperative and perioperative outcomes of robotic (RASP) and laparoscopic (LSP) simple prostatectomy.
Methods: We retrospectively analyzed data from patients who underwent minimally invasive simple prostatectomy at the Urological Department of Portogruaro Hospital, Portogruaro, and at the Urological Department of “San Bassiano” Hospital, in Bassano del Grappa, from March 2015 to December 2020. Data collected from medical records included age, body mass index, prostate volume, operative time, preoperative International Prostatic Symptoms Score (IPSS), postoperative IPSS, time with drainage, blood transfusion, intraoperative complications, perioperative complications and length of hospital stay.
Results: Robotic-assisted (n = 25) and laparoscopic simple prostatectomy (n = 25) were performed with a transvesical approach. No significant differences were observed regarding baseline characteristics, body mass index, prostate volume and IPSS. Operative time was lower in the laparoscopic group (122 min vs 139 min) (p = 0.024), while hospital stay was lower in the robotic group (4 days vs 6 days) (p = 0.047).
Conclusions: Robotic-assisted simple prostatectomy is a safe technique with results comparable to laparoscopic simple prostatectomy, encompassing the advantage of a shorter hospitalization. Considering the costs and the limited availability of robotic-assisted simple prostatectomy, laparoscopic simple prostatectomy is a valid and safe alternative for experienced surgeons.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/aiua.2022.1.37
https://doi.org/10.4081/aiua.2022.1.37



