Perspectives on the urological care in Parkinson’s disease patients
Accepted: January 6, 2022
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
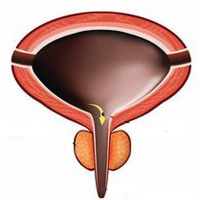
Parkinson's disease (PD) is recognized as the most common neurodegenerative disorder after Alzheimer's disease. Lower urinary tract symptoms are common in patients with PD, either storage symptoms (overactive bladder symptoms or OAB) or voiding symptoms. The most important diagnostic clues for urinary disturbances are provided by the patient's medical history. Urodynamic evaluation allows the determination of the underlying bladder disorder and may help in the treatment selection. Pharmacologic interventions especially anticholinergic medications are the first-line option for treating OAB in patients with PD. However, it is important to balance the therapeutic benefits of these drugs with their potential adverse effects. Intra-detrusor Botulinum toxin injections, electrical stimulation were also used to treat OAB in those patients with variable efficacy. Mirabegron is a β3-agonist that can also be used for OAB with superior tolerability to anticholinergics. Desmopressin is effective for the management of nocturnal polyuria which has been reported to be common in PD. Deep brain stimulation (DBS) surgery is effective in improving urinary functions in PD patients. Sexual dysfunction is also common in PD. Phosphodiesterase type 5 inhibitors are first-line therapies for PD-associated erectile dysfunction (ED). Treatment with apomorphine sublingually is another therapeutic option for PD patients with ED. Pathologic hypersexuality has occasionally been reported in patients with PD, linked to dopaminergic agonists. The first step of treatment of hypersexuality consists of reducing the dose of dopaminergic medication. This review summarizes the epidemiology, pathogenesis, risk factors, genetic, clinical manifestations, diagnostic test, and management of PD. Lastly, the urologic outcomes and therapies are reviewed.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/aiua.2022.1.107
https://doi.org/10.4081/aiua.2022.1.107



