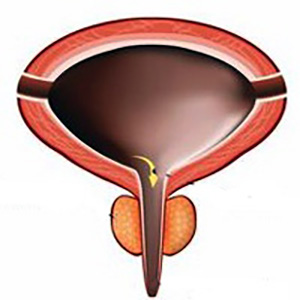
Outcomes of continent and incontinent external urinary diversion in management of patients with refractory non-malignant lower urinary tract dysfunction
Accepted: November 25, 2022
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
Objective: To evaluate the early and late outcomes of continent and incontinent external urinary diversion in management of patients with refractory non-malignant lower urinary tract dysfunction (LUTD).
Materials and methods: The charts of patients with refractory non-malignant LUTD who underwent continent or incontinent external urinary diversion at University of Cincinnati hospitals in the period between March 2012 and December 2019 were retrospectively reviewed. The demographic and baseline characteristics, surgery indications, operative data, early and late outcomes were collected, analyzed, and compared.
Results: A total of 78 patients including 55 patients with neurogenic bladder (NGB) and 23 patients with non-neurogenic bladder (non-NGB) refractory non-malignant LUTD were included. Fifty-three patients underwent incontinent urinary diversions (IUD), while 25 patients underwent continent urinary diversions (CUD). During the first 4 postoperative weeks, 53.85% (n=42) of patients developed complications, and the incidence was nonsignificantly higher in patients with NGB than those with non- NGB (56.36% vs 47.83%, p-value=0.490). Fever was exclusively encountered in patients with NGB earlier, while stomal retraction occurred only in patients with non-NGB later. More non- NGB patients had early wound infection. There was an overall improvement of urological symptoms in 52 patients (66.67%), and the rate was non-significantly higher in non-NGB patients than NGB patients (78.26% vs 61.82%, p-value=0.160). Late complications were reported in 47 patients and were more encountered in those with non-NGB than those with NGB (65.22% vs 58.18%). Stomal leakage and stenosis occurred more with CUD than with IUD (52% vs 0% and 28% vs 3.77%, respectively).
Conclusions: External urinary diversion can achieve a reasonable level of urological symptoms control in patients with refractory non-malignant LUTD, but with associated adverse outcomes. Although non-significantly, these complications tend to be higher in patients with IUD and/or NGB during the early postoperative period and higher with CUD and/or non-NGB on the long-term.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/aiua.2022.4.384
https://doi.org/10.4081/aiua.2022.4.384



