Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
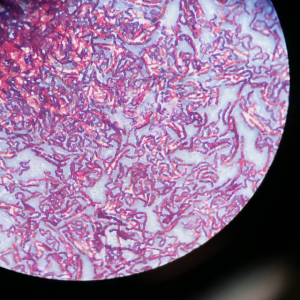
A comparative evaluation of colistin Minimum Inhibitory Concentration determination by reference broth microdilution with other commonly used phenotypic methods in Multidrug-Resistant Gram-negative bacilli
Background: over the past decade, the dependency on colistin as a last resort antibiotic has driven the global emergence of colistin resistance among many bacterial species. This study comparatively evaluated the colistin Minimum Inhibitory Concentration (MIC) by various phenotypic methods, including the reference method of Broth Microdilution (BMD), other approved methods of Colistin Broth Disk Elution (CBDE), and Colistin Agar Test (CAT) and widely available method of Epsilometer Test (E-test) among Multidrug Resistant (MDR) Gram-negative bacteria. Methods: ninety Gram-negative bacterial isolates that were resistant to three or more classes of drugs (MDR) were included in the study. All the MDR isolates were subjected to colistin susceptibility determination by BMD, CBDE, CAT, and E-test. Results: amongst 1118 samples, 90 (8.05%) samples yielded MDR Gram-negative bacilli. All the MDR Gram-negative isolates were colistin intermediate by all four methods of phenotypic colistin susceptibility. Three Acinetobacter baumannii and two Klebsiella pneumoniae isolates that had MIC of 2 μg/mL by BMD, displayed MIC of <1 μg/mL by CBDE and CAT. Three isolates (2 Citrobacter koseri and 1 Enterobacter spp.) showed higher MIC by the E-strip method in comparison to BMD. Conclusions: our study holds significance, as there is a paucity of data comparing the four phenotypic methods for colistin MIC determination; BMD is the most reliable, gold standard method, but it is labor-intensive and requires technical expertise. In the present study, CBDE and CAT methods showed good concordance with BMD, and are easy to perform with limited logistics. Thus, they can be used as an alternative to BMD. We found that even though the Etest method was less accurate, it can still be used with caution to exclude the possibility of colistin resistance.
Downloads
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/mm.2023.11573
https://doi.org/10.4081/mm.2023.11573