Patterns of Mannose-Binding Lectin (MBL) responses to Plasmodium falciparum infections in hyperendemic settings
Accepted: 28 September 2023
HTML: 20
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
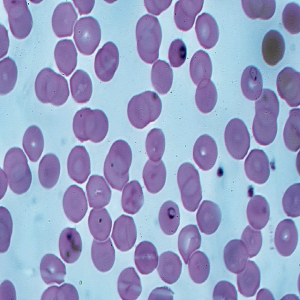
Background: malaria caused by Plasmodium falciparum remains a significant and major public health concern in Africa, particularly in hyperendemic regions. Recurrent fevers and high quantities of inflammatory mediators in the circulation define the disease's blood stages. By binding to non-self-pathogen oligosaccharide surfaces, Mannose-Binding Lectin (MBL) and lectin complement pathways trigger innate immune processes and contribute to the formation of adaptive immune responses. Methods: in Sudan, we investigated the varied immune response levels of MBL to the different phases of P. falciparum infection in White Nile and Blue Nile states endemic to malaria. And we looked at the interaction of regulatory Interleukin 6 (IL- 6) cytokines on MBL during infection. Our study was based on a total of 108 cases, in which 86 patients (62.0%) were uncomplicated and (17.6%) were severe, all met the diagnostic criteria and were clinically admitted for malaria infections. For the determination of serum MBL and IL-6 levels, a commercial ELISA kit was employed. Results: the analysis of the results revealed significantly elevated levels of MBL and IL-6 in both severe and uncomplicated cases (p<0.001). And MBL average in contrast to residents, Blue Nile patients had high parasitemia (599.9 ng/mL) and this difference was statistically significant (p-value<0.05). The remarkable positive correlation of IL-6 serum levels with MBL among malaria patients and healthy controls (r=0.399, p<0.001) was noted too. Conclusions: according to the findings of this study, patients living in hyperendemic areas exhibit a different MBL response rate and appear to be more homogeneous in proportion to the density of P. falciparum due to parasitemia. In addition, it is also dependent on the regulatory immune mediator IL-6.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/mm.2023.11517
https://doi.org/10.4081/mm.2023.11517



