Omega-3 PUFAs and gut microbiota: A preventive approach for colorectal cancer
Accepted: November 20, 2021
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
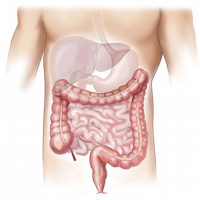
The influence of diet on the composition of the intestinal microbiota and related pathologies has been known for some time. Some classes of nutrients, such as fatty acids belonging to the omega 3 series, have particular effects on the bacteria that make up the intestinal microbiota. ω-3 PUFAs affect the gut microbiota in three different ways: by modulating the type and abundance of intestinal bacteria, by regulate SCFAs levels, and by alter the levels of proinflammatory mediators. Through these modalities, ω-3 PUFAs could be useful for the prevention of intestinal diseases such as Colorectal Cancer (CRC). The ability of ω-3 PUFAs to modulate the intestinal inflammatory response, to preserve the integrity of the intestinal mucosa and to modulate the bacterial composition of the intestine, could be useful as a preventive strategic approach to hinder the development of CRC.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/jbr.2021.9954
https://doi.org/10.4081/jbr.2021.9954



