Different diagnostic strategies for different settings
Accepted: 17 February 2021
HTML: 315
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
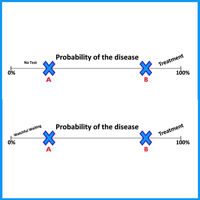
Diagnostic strategies should always take into consideration the setting in which they are administered. The predictive value, positive or negative of a clinical sign or diagnostic test has a different weight in family medicine than in the hospital setting. Many tests have not been formally evaluated in primary care; unfortunately, very often low prevalence settings are used to conduct screening in these populations, and often result in unrealistically high prevalence estimates for chronic disease and these results are then used to conclude that General Practitioners are not good at detecting diseases. In primary care, the prevalence and incidence of disease differs from what appears in the hospital setting, and severe disease occurs less frequently in general practice than in hospital because there is no preventive selection. This requires a specific probability-based decision-making process, based by the knowledge of patients and the community. In primary care, the diagnostic strategy should begin with complaints and symptoms and address uncertainty and complexity, using step-by-step strategies, including watchful waiting, presumptive symptomatic treatment, and focusing on low-tech strategies.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/gc.2021.9538
https://doi.org/10.4081/gc.2021.9538



