Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
A serious fit of cough: A 66-year-old patient with myasthenia gravis presenting with spontaneous intercostal lung herniation after coughing. Case report and pathophysiological discussion
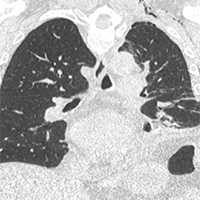
We present a case of a 66-year-old man with history of myasthenia gravis, severe obesity and osteopenia self-presented to our Emergency Department (ED) with severe pain in his left hemithorax, occurred after an episode of cough three days before. No history of trauma was reported. The patient underwent a chest-XR showing uncomplicated spontaneous fractures of the 5th and 6th left ribs. He was therefore discharged with appropriate analgesic treatment. Five days later, the patient came back to our ED for a wide left abdominal hematoma, though hemodynamically stable and eupneic. A CT-scan with contrast showed a rare and unexpected spontaneous left intercostal lung herniation complicated with a diffuse subcutaneous emphysema, pneumothorax, loculated bilateral pleural effusion and abdominal hematoma. The patient was admitted, treated conservatively and safely discharged after two weeks. We also provide a pathophysiological discussion of the case and a literature review.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ecj.2020.8911
https://doi.org/10.4081/ecj.2020.8911