Evaluation of paraclinical methods in diagnosis of Foreign Body and its complications compared to operating room findings in patients with oral, pharyngeal and esophageal symptoms in Amir A’lam Hospital
Accepted: 28 February 2020
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
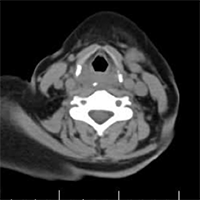
Foreign Body (FB) swallowing is one of the most common medical emergencies in the world. This injury can cause mortality and morbidity in all age groups. This study aimed to evaluate the paraclinical methods in diagnosis of foreign body and its complications compared to operating room findings in patients with oral, pharyngeal and esophageal symptoms. This was a retrospective study. All patients referred to the ENT (Ear, Nose, Throat) department of Amir A’lam hospital with complaints of foreign body swallowing admitted in the operating room were studied. The patients’ information including demographic information, type of swallowed body, paraclinical information and operating room findings were extracted from the patients’ records. This study was performed on 219 patients admitted to ENT clinic. The mean age of the patients was 45.10±20.61 years. The highest and the lowest frequencies for foreign body type were chicken bone in 61 cases (28.31%) and disk battery in 1 case (0.5%). The most and the least frequency of complaints after foreign body type were dysphagia in 129 cases (58.9%) and neck tenderness in 7 cases (3.19%). Computerized Tomography (CT) scan findings and operative findings were almost same except in two cases. Kappa agreement for lateral neck and observation in the operating room was 50.5% (P <0.001) and WBC count was significantly higher in patients with complications (P=0.010).
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ecj.2020.8726
https://doi.org/10.4081/ecj.2020.8726








