Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Changes in kinesiostabilogram parameters and movement speed of stroke patients while increasing their physical activity due to the use of biofeedback method
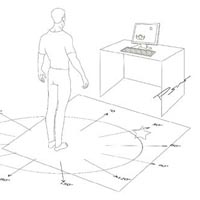
Balance disorders are complications of stroke survivors. Aim of this study was the establish effectiveness of the biofeedback approach. In this intervention study 245 patients with early diagnosis of acute disturbance of cerebral circulation (ADCC) were examined. Patients able to move independently were treated by standard conservative ADCC therapy on an outpatient approach, but they continued to have problems with coordination of movement in upright position. Then they were submitted to an increasing physical activity based on five sessions of biofeedback, i.e., a complex rehabilitation of patients with motor pathology "Trust-M" according to TU 9442-001-63704475-2010. Mobility rates were assessed using a web camera. Patients' quality of life was evaluated by SF-36 questionnaire and the Hospital Anxiety and Depression Scale (HADS). All parameters were recorded before and after 5 sessions of biofeedback. After treatment, the stability indicators improved and all patients showed a significant increase in motion rate and quality of life. At the same time, the severity of pain and of depression and anxiety decreased. Negative correlations of average strength between the quadrant and patient HADS scaling rates were obtained. In conclusion, our work shows effectiveness of the biofeedback technique for correcting coordination in stroke survivors.
Downloads
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2021.9360
https://doi.org/10.4081/ejtm.2021.9360