Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Balance and muscle strength tests in patients with osteoporotic vertebral fractures to develop tailored rehabilitation programs
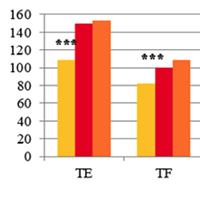
Authors perform a cross-sectional study of functional abilities of the patients with osteoporotic VF. Trunk muscle isometric strength and balance impairments were estimated. The development of osteoporotic VFs is associated with a significant decrease in strength of all the body muscles, especially the deep spinal stabilization system (TE, TF), where the VFs contribute to inappropriate distribution of back muscle strength with TE:TF ration of 1:1 instead of 3:2, observed both normally and in patients with uncomplicated osteoporosis. There is also a deterioration of stabilometry and functional balance assessment tests in patients with pathological VFs, which indicates abnormalities of both static and dynamic balance. The obtained data should be taken into account when developing rehabilitation programmes for patients with osteoporosis who have suffered compression VFs.
Downloads
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2020.9236
https://doi.org/10.4081/ejtm.2020.9236