Sporadic late onset nemaline myopathy with monoclonal gammopathy of undetermined significance: two cases with long term stability
Accepted: 2 August 2020
HTML: 58
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
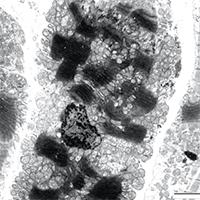
Monoclonal gammopathy of undetermined significance (MGUS) associated to sporadic late onset nemaline myopathy (SLONM) is a rare and severely disabling condition of quickly progressive limb girdle acquired myopathy. It is believed by some authors to be due to myotoxicity of light chain deposits. Two female patients were diagnosed with MGUS associated SLONM. In the first case, diagnosis was delayed by 6 years thus giving time for a severe generalized myopathy and cardiomyopathy to develop. A single anti-myeloma chemotherapy with lenalidomide markedly improved and stabilized the patient’s condition despite respiratory and cardiac insufficiency. In our second patient the condition was identified one year after onset of the first symptom and markedly improved after autologous bone marrow transplantation and lenalidomide. Clinicians should be aware of monoclonal gammopathy associated sporadic late onset nemaline myopathy as this acquired muscle disorder, although extremely rare, may be reversed by adequate management.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2020.9225
https://doi.org/10.4081/ejtm.2020.9225



