Diminution in sperm quantity and quality in mouse models of Duchenne Muscular Dystrophy induced by a myostatin-based muscle growth-promoting intervention
Accepted: 12 March 2020
HTML: 50
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
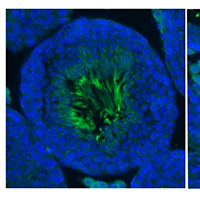
Duchenne Muscular Dystrophy is a devastating disease caused by the absence of a functional rod-shaped cytoplasmic protein called dystrophin. Several avenues are being developed aimed to restore dystrophin expression in boys affected by this X-linked disease. However, its complete cure is likely to need combinational approaches which may include regimes aimed at restoring muscle mass. Augmenting muscle growth through the manipulation of the Myostatin/Activin signalling axis has received much attention. However, we have recently shown that while manipulation of this axis in wild type mice using the sActRIIB ligand trap indeed results in muscle growth, it also had a detrimental impact on the testis. Here we examined the impact of administering a powerful Myostatin/Activin antagonist in two mouse models of Duchenne Muscular Dystrophy. We report that whilst the impact on muscle growth was not always positive, both models showed attenuated testis development. Sperm number, motility and ultrastructure were significantly affected by the sActRIIB treatment. Our report suggests that interventions based on Myostatin/Activin should investigate off-target effects on tissues as well as muscle.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2020.8904
https://doi.org/10.4081/ejtm.2020.8904



