Dental implants in Sjögren syndrome
Accepted: 16 February 2020
HTML: 116
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
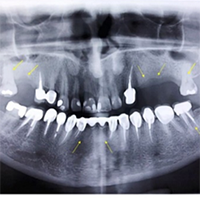
Sjögren's syndrome (SS) is a complex autoimmune disease that predominantly affects the exocrine glands, notably the salivary and lacrimal glands, resulting in dryness of the mucosa recognized as xerostomia. Chief oral complications reported by patients consist of high caries rate, burning sensation of the mucosa, early tooth loss, intensified tooth wear and repetitive failure of dental restorations. In particular, due to the decreased salivary flow, conventional removable prostheses might irritate the mucosa and lead to painful ulcerations at the borders of the denture. Implant-supported prostheses offer a unique solution to the difficulties experienced by edentulous patients with Sjögren’s syndrome. This research showed no signs of peri-implantitis or peri-implant mucositis during 7-years following the placement of implants. The present study indicates that successful long-term maintenance of dental implants can be also achieved in SS patients.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2020.8811
https://doi.org/10.4081/ejtm.2020.8811



