Motion sickness susceptibility and visually induced motion sickness as diagnostic signs in Parkinson’s disease
Accepted: 6 October 2022
HTML: 11
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
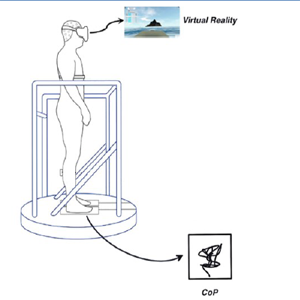
Postural instability and loss of vestibular and somatosensory acuity can be part of the signs encountered in Parkinson’s Disease (PD). Visual dependency is described in PD. These modifications of sensory input hierarchy are predictors of motion sickness (MS). The aim of this study was to assess MS susceptibility and effects of real induced MS in posture. 63 PD patients, whose medication levels (levodopa) reflected the pathology were evaluated, and 27 healthy controls, filled a MS questionnaire; 9 PD patients and 43 healthy controls were assessed by posturography using virtual reality. Drug amount predicted visual MS (p=0.01), but not real induced MS susceptibility. PD patients did not experience postural instability in virtual reality, contrary to healthy controls. Since PD patients do not seem to feel vestibular stimulated MS, they may not rely on vestibular and somatosensory inputs during the stimulation. However, they feel visually induced MS more with increased levodopa drug effect. Levodopa amount can increase visual dependency. The strongest MS predictors must be studied in PD to better understand the effect of visual stimulation and its absence in vestibular stimulation.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.
Similar Articles
- Sandra Zampieri, Ines Bersch, Piera Smeriglio, Elena Barbieri, Simona Boncompagni, Maria Chiara Maccarone, Ugo Carraro, Program with last minute abstracts of the Padua Days on Muscle and Mobility Medicine, 27 February – 2 March, 2024 (2024Pdm3) , European Journal of Translational Myology: Vol. 34 No. 1 (2024)
- Sandra Zampieri, Ines Bersch, Piera Smeriglio, Elena Barbieri, Massimo Ganassi, Christiaan Leeuwenburg, Riccardo Rosati, Paolo Gargiulo, Amber Pond, H. Lee Sweeney, Ugo Carraro, Five Padua days on muscle and mobility medicine (2024Pdm3) 27 February - 2 March, 2024 at Hotel Petrarca, Thermae of Euganean Hills, Padua, and San Luca Hall, Prato della Valle, Padua, Italy , European Journal of Translational Myology: Vol. 33 No. 4 (2023)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejtm.2022.10884
https://doi.org/10.4081/ejtm.2022.10884



