HIV infection and increased risk of COVID-19 mortality: A Meta-Analysis
Accepted: 4 October 2021
HTML: 8
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
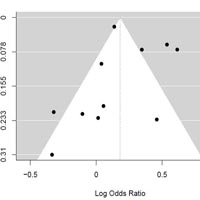
There are some concerns on the effect of infection with human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) on the outcome and mortality of COVID-19. In this meta-analysis, we aimed to address this issue and assess the risk of mortality in COVID-19 patients who are co-infected with HIV. Two International electronic databases (PubMed, Scopus) were searched from the first time available to 12 August 2021. The targeted outcome was the pooled odds ratio to examine the effect of HIV infection on COVID-19 mortality. The crude odds ratio (OR) for all studies and the pooled OR were calculated with 95% confidence interval. The forest plot was used to graphically represent the result of conducted meta-analysis and calculated OR for individual studies. The I2 statistic was used to examine the Heterogeneity in the included studies. Eleven studies were included in our study consisting of 19,642,775 COVID-19 infected cases, 59,980 HIV-positive, and 4,373 deaths due to COVID-19 in HIV positive patients. The overall pooled odds ratio was 1.21 (CI: 1.02; 1.43) and P-value < 0.0277. The I^2 value was 89% (P-value < 0.0001), which shows that included studies are heterogeneous. In this study, the funnel plot analysis showed symmetry among the included studies. HIV-positive patients are 21% more likely to die because of COVID-19 infection than people without HIV. Special attention should be considered for the prevention and treatment of COVID-19 and consistent treatment for HIV infection, in HIV-positive patients.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2021.10107
https://doi.org/10.4081/ejtm.2021.10107



