Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
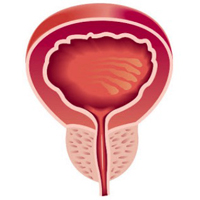
The presence of chronic inflammation in positive prostate biopsy is associated with upgrading in radical prostatectomy
Objective: This study aimed to determine the predictive effect of the presence of chronic prostatitis associated with prostate cancer (PCa) in prostate biopsy on Gleason score upgrade (GSU) in radical prostatectomy (RP) specimens.
Materials and methods: The data of 295 patients who underwent open or robotic RP with a diagnosis of localized PCa following biopsy were retrospectively analyzed. Patients were divided into two groups with and without GSU following RP. Predictive factors affecting GSU on biopsy were determined. The impact of chronic prostatitis associated with prostate cancer on GSU was examined via logistic regression analysis.
Results: Out of 224 patients with Gleason 3+3 scores on biopsy, 145 (64.7%) had Gleason upgrade, and 79 (35.2%) had no upgrade. Whilst comparing the two groups with and without Gleason upgrade in terms of patient age, prostate-specific antigen (PSA) value, PSA density (PSAD), prostate volume (PV), neutrophil/lymphocyte (N/L) ratio, number of positive cores, percentage of positive cores, and Prostate Imaging Reporting and Data System version 2 score, no statistically significant difference was detected. The presence of chronic prostatitis associated with PCa was higher in the patient cohort with GSU in contrast to the other group (p < 0.001). According to the univariate logistic regression analysis, the presence of chronic prostatitis was identified to be an independent marker for GSU.
Conclusions: Pathologists and urologists should be careful regarding the possibility of a more aggressive tumor in the presence of chronic inflammation associated with PCa because inflammation within PCa was revealed to be linked with GSU after RP.
Downloads
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/aiua.2021.3.280
https://doi.org/10.4081/aiua.2021.3.280