The prevalence and management of obstetric fistula among women of reproductive age in a low-resource setting
Accepted: 20 September 2023
HTML: 39
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
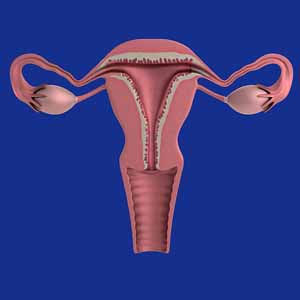
Obstetric fistula is one of the most significant obstetrical concerns and apparent indications of maternal morbidity in low-resource nations. Therefore, the study assessed the prevalence and management of fistula among women of reproductive age (15-49) in low-resource settings. This population-based cross-sectional study was conducted in three local government areas (Jere, Konduga and Maiduguri Municipal City) in Borno State. A structured questionnaire was used to collect data from 484 respondents, and the data were analysed using SPSS version 25.0. The overall prevalence of obstetric fistula was 10.7%. Over 13% of women with seven or more vagina deliveries had a fistula. Likewise, 19% of respondents knew about fistula prevention and treatment services available, and 13.7% of those did not participate in antenatal care services. Furthermore, 48.1% of respondents with a fistula during labour were treated successfully. Almost half (47.9%) who were aware of health facilities around them were successfully treated, same with 46.2% of those living within 1 to 2 km of a health facility, and almost half (49.0%) of those who got married within age 20. The study emphasizes the importance of effective community-level interventions to address obstetric fistula. To achieve this, a comprehensive action plan should be developed, ensuring pregnant women have access to necessary obstetric care services at all healthcare levels. The plan should include preventive measures, timely management of labour complications, and increased awareness of fistula prevention and treatment services. Prioritizing maternal healthcare and empowering women with knowledge and access to services are essential in preventing and managing obstetric fistula.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.

 https://doi.org/10.4081/hls.2023.11566
https://doi.org/10.4081/hls.2023.11566



