Clinical manifestation and microbial profiling of recurrent MDR microorganisms associated with head and neck infection- a retrospective study
Accepted: 28 July 2023
HTML: 5
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
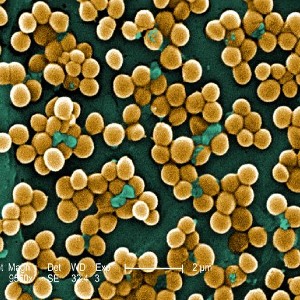
Head and neck infection (HNI) can lead to life-threatening complications, including death. The purpose of this study is to look at the entire clinico-demographic profile of patients with HNI as well as the microbiologic profile of recurring bacterial infection cases with a variety of symptoms. A retrospective cross-sectional study was conducted on 1080 HNI patients in a tertiary care hospital in Bhubaneswar, Odisha, India, from January 2018 to December 2022. Of the 1080 cases, 771 (71.39%) were males, 309 (28.61%) were females, and 603 (55.83%) were from rural areas reporting to a tertiary care hospital. 62% of the cases were between the ages of 31 and 60. Neck abscesses account for 570 (52.78%) of all cases, with parotid abscesses accounting for 233 (21.57%), peritonsillar abscesses accounting for 170 (15.74%), otitis media 32 (2.96%), and oral cavity infection accounting for 26 (2.41%). In 854 (79.07%) cases, the etiology was odontogenic, followed by sinus in 188 (17.41%) and otogenic in 38 (3.52%). The most common presenting features were neck swelling in 537 (49.72%) cases and face swelling in 238 (22.04%) cases, followed by jaw pain in 26 (2.41%) cases and others. Patients were hospitalized for an average of 11.824.38 days. Treatment and recurrence had a strong significant relationship (p 0.001). Microbiologic investigation of recurrent patients revealed 12 microorganisms, including bacteria and fungus, mainly multidrug-resistant in given ascending order Staphylococcus aureus (26.74%), Klebsiella pneumoniae, Pseudomonas aeruginosa, Acinetobacter baumannii, Escherichia coli, Candida albicans (4.65%), Aspergillus fumigatus, A. flavus, A. niger, C. tropicalis, C. glabrata, C. krusei. Apart from colistin, almost all antibiotics were highly resistant to gram-negative bacteria, whereas against S. aureus, benzylpenicillin, and oxacillin showed 100% resistance, followed by erythromycin (91.3%), levofloxacin (86.96%), and ciprofloxacin (82.61%). This exploratory study would aid in determining the HNI burden and epidemiology, as well as their treatment status.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.

 https://doi.org/10.4081/hls.2023.11527
https://doi.org/10.4081/hls.2023.11527



