Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
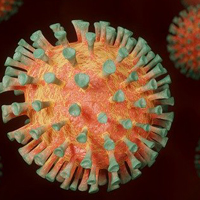
Steroids in severe COVID-19 patients: A retrospective analysis on the first pandemics in Lombardy
The pathogenesis of COVID-19 appears to be characterized by a dysregulated immune response. During the first pandemic wave in Lombardy, we started to administer glucocorticoids to some patients with severe respiratory failure requiring support with Continuous Positive Airway Pressure (CPAP) therapy. We retrospectively collected data to identify the effect of glucocorticoids in this COVID-19 particular population. With a multidisciplinary consensus, we administered to selected patients with severe COVID-19 disease (PaO2/FiO2 159±71 mmHg) 0,91 mg/kg/die of methylprednisolone equivalent dose after a median of 8 days of hospitalization. In our study we compared 57 patients from the steroid group with 123 from the control group: the event of invasive mechanical ventilation or death was reduced by 43% between steroid group and control group (19.3 % vs. 34.1 % respectively, p=0.001) and mortality was reduced by about 31% between steroid and usual care alone (15.8 % vs. 22.8 % respectively, p=0.011). Corticosteroids in selected COVID-19 patients may have a relevant impact on outcome, better profiling of the heterogeneity of this disease may be essential to guarantee the best treatment choices.
Downloads
Citations
10.4081/ecj.2021.10139
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ecj.2021.9888
https://doi.org/10.4081/ecj.2021.9888