Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
SARS-CoV-2 management in Emergency Department: risk stratification and care setting identification proposal based on first pandemic wave in Pisa University Hospital
SARS-CoV-2 management in Emergency Department: risk stratification and care setting identification proposal based on first pandemic wave in Pisa University Hospital
Background: COVID-19 patients require early treatment and admission to an appropriate care setting, considering possible rapid and unpredictable to Severe Acute Respiratory Syndrome.
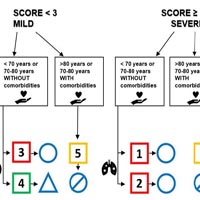
Objective: A flow-chart was developed by a multidisciplinary team of Emergency Department (ED) clinicians, intensivists and radiologists aiming to provide tools for disease severity stratification, appropriate ventilation strategy and hospitalization setting identification.
Methods: We conducted a retrospective application of our model on 313 hospitalized patients at Pisa University Hospital including 222 patients admitted to ED for respiratory failure between March and April 2020. Risk stratification score was based on respiratory and chest imaging parameters, while management strategy on comorbidities and age.
Results: Age, comorbidities, clinical respiratory and arterial blood gas parameters, semi-quantitative chest computed tomography score were significant predictors of mortality (p<0,05). Mortality rate was higher in patients treated in intensive care units (26,5%) and undergoing endo-tracheal intubation (32,7%), compared to medical area (21,3%). We verified a good concordance (81,7%) between the proposed model and actual evaluation in ED. Outcomes analysis of subgroups of patients homogeneous for baseline features allowed to verify safety of our model: in non-elderly and/or non-comorbid patients (15% mortality) our scheme overestimates the risk in 30% of cases, but it suggests non-intensive management in patients with reduced functional reserve, elderly and with comorbidities (50% mortality).
Conclusion: Correct management of respiratory failure COVID-19 patients is crucial in this unexpected pandemic. Our flow-chart, despite retrospectively application in small sample, could represents a valid and safe proposal for evaluation in ED.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ecj.2021.9859
https://doi.org/10.4081/ecj.2021.9859