Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Can Left ventricular outflow tract aortic velocity time integral guide fluid resuscitation in septic patients? - A case report
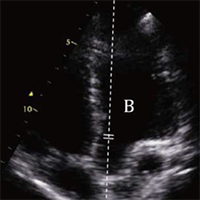
Hemodynamic monitoring of unstable patients is an everyday issue for Emergency Physicians (EP). Considering the difficulty, in Emergency Department (ED) settings, to assess invasively Stroke Volume (SV), Cardiac Output (CO) and Peripheral Vascular Resistance (PVR), EP should be familiar with non-invasive, easy and reproducible methods that can estimate these parameters. The use of Left Ventricular Outflow Tract aortic Velocity Time Integral (LVOT-VTI) with echocardiography, as estimate of SV, integrated with inferior vena cava collapse index and clinical examination could give the opportunity to non-invasively understand at which point of an ideal cardiac output/central venous pressure relation (according to the Frank Starling law) the patient is situated. In this case report we describe a septic patient accessing the ED with both respiratory and cardiac failure, and we show that the use of aortic LVOT-VTI is an easy and reproducible approach to understand cardiac hemodynamic in scenarios involving multiple pathologic mechanisms.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ecj.2020.8817
https://doi.org/10.4081/ecj.2020.8817