Unraveling the intricacies of acute temporomandibular joint dislocation in emergency department: a multidimensional exploration of reduction techniques and success rate by emergency physicians
Accepted: 4 October 2023
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
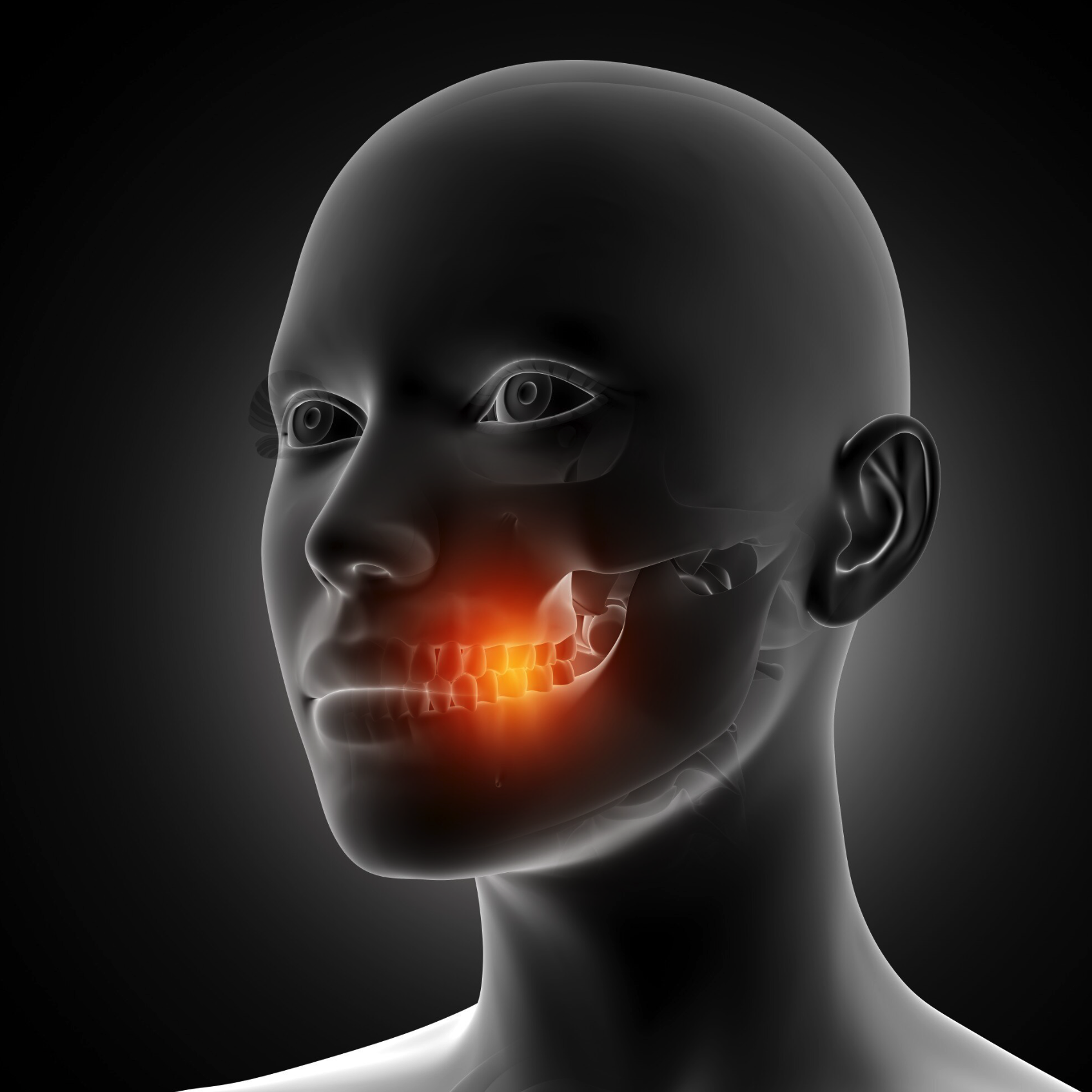
Temporomandibular joint (TMJ) dislocation is a distressing condition that requires prompt management in the emergency setting. This retrospective study aimed to assess the success rate of TMJ reduction performed by emergency physicians (EPs) and evaluate the commonly used reduction techniques and sedative choices. The EPs achieved an overall success rate of 86.29% in reducing the dislocations. Among the successful reductions, 68.21% were accomplished in the first attempt, with only 7.29% requiring three or more attempts. Procedural sedation and analgesia were commonly employed, with midazolam (34.44%) and fentanyl (21.85%) being the most frequently used in successful cases. The Classic intraoral technique (29.14%) was the preferred method for successful reductions. No significant differences were observed in drug utilization or reduction techniques between the groups of successful and failed reductions. The findings demonstrate the high competence of EPs in managing acute TMJ dislocations in the emergency department. The study provides valuable insights into the commonly employed reduction techniques and sedative choices, offering important guidance for emergency medical practice.
Edited by
NilSupporting Agencies
NilHow to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ecj.2023.11643
https://doi.org/10.4081/ecj.2023.11643








