Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Challenges of the next generation hospitals: Rethinking the Emergency Department
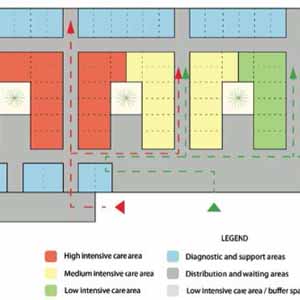
The COVID 19 outbreak dramatically highlighted the inadequacy of the Emergency Department (ED) settings in dealing with events that can acutely affect a wide range of population. The immediate urgency to create strictly distinct pathways became also a strategic aspect for reducing possible sources of contagion inside the hospital.1 This need has often clashed with inadequate structural conditions of the hospital: in fact, the rigidity of many EDs is due to the hospital typology and its localization (affected by functional program);2,3 and it prevents them from being quickly adapted to new needs in the case of maxi-emergencies.4 In several recent international projects, the presence of a multifunctional space and/or a buffer area guarantees different scenarios in relation to the healthcare/emergency needs.5 [...]
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ecj.2022.10840
https://doi.org/10.4081/ecj.2022.10840