Delayed splenic rupture after a minor blunt trauma: A case report and literature review
Accepted: 1 September 2022
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
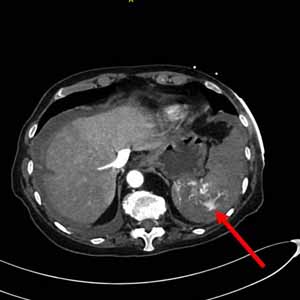
Delayed Splenic Rupture (DSR) is a rare but well-known manifestation of Blunt Splenic Injury (BSI), which most commonly occurs following a car accident, a fall from a great height, or a direct blow to the left thorax or abdomen. If the history of trauma is remote or unknown, the diagnosis can be difficult or missed, and a high index of suspicion is not warranted. Regardless of the time and mechanism of the inciting event, DSR should be considered in the differential diagnosis of an acute surgical abdomen. We present a case of DSR in an 81-year-old woman caused by a remote minor blunt abdominal trauma four weeks prior to her admission to our emergency department for acute abdominal pain and hemorrhagic shock (ATLS CLASS III). Starting with this case report, we conducted a literature review on the subject in order to raise awareness, knowledge, and understanding of DSR among emergency clinicians.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ecj.2022.10822
https://doi.org/10.4081/ecj.2022.10822








