Open thoracotomy and decortication for chronic empyema thoracis: Our experience
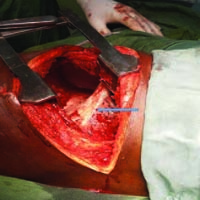
Empyema thoracis is defined as the presence of pus in the pleural space or a purulent pleural effusion. Chronic empyema is characterized by thickened visceral and parietal peels, which hamper the ability of the affected lung to re-expand and require definitive surgical intervention. In a resource constraint environment like ours, open thoracotomy and decortication is the treatment of choice. We review our experience with cases of chronic empyema thoracis that had thoracotomy and decortication. This is a descriptive, retrospective, and observational study. Medical records of patients who had thoracotomy and decortication on account of chronic empyema thoracis in the Cardiothoracic surgery unit of our hospital between 2012 and 2020 were retrieved and reviewed. The information obtained from the records included sex, age, premorbid conditions, aetiology of empyema, cultures of pleural fluids, histology results of the cortex removed, duration of chest tube drainage, duration of hospital stay, postoperative complications, and outcome. One hundred and eighty-five patients diagnosed with empyema thoracis were seen in the study period. Sixty-five patients had thoracotomy and decortication on account of chronic empyema thoracis while the remaining 120 (64.9%) had closed tube thoracostomy drain insertion. Male: female was 5:1, mean age at presentation 24.24 years with age ranging from 2 years to 70 years. Fourteen (23.33%) were in the paediatric age group while the remaining (76.67%) were adults. The aetiology of empyema was pneumonia in 36 (60%). Strept pneumoniae was the commonest organism isolated from pleural fluids of these patients accounting for 23.33%. All patients underwent thoracotomy and decortication. The mean duration before surgery was 17 days with a range of 2 days to 40 days. The average duration of surgery was 2 hours. Chest tube was removed after an average of 7 days (range 5 to 33 days. Twenty-one patients (35%) had complications. The average duration of drainage was 18.87 days and that of hospital stay was 36.74 days. There were 3 mortalities (5%). The mean duration of follow-up was 3 months. Chronic empyema thoracis is still common in our environment and presentation is usually very late. In our series, open thoracotomy and decortication was found to be an excellent procedure with low morbidity and mortality. The majority of our patients had good functional outcome with few complications.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/cdr.10.9844
https://doi.org/10.4081/cdr.10.9844