Impact of exercise training on the sarcopenia criteria in non-alcoholic fatty liver disease: a systematic review and meta-analysis
Accepted: 7 February 2021
Supplementary Materials: 0
HTML: 17
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
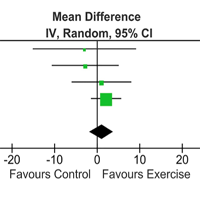
Authors
Sarcopenia is a highly prevalent complication of non-alcoholic fatty liver disease (NAFLD). We aimed to conduct a systematic review and meta-analyses to elucidate the exercise training (ET)'s efficacy on NAFLD adult patients' sarcopenia criteria. We identified relevant randomized controlled trials (RCT) in electronic databases PubMed, CINAHL, and Scopus. We selected seven RCT from 66 screened studies. The ET programs included endurance or combined (endurance and resistance) training. No study performed resistance training alone. The physical function improved with endurance or combined training (mean differences [MD] 8.26 mL/Kg*min [95% CI 5.27 to 11.24 mL/Kg*min], p < 0.0001); Muscle mass showed no evidence of the beneficial effects of endurance or combined training (MD 1.01 Kg [95% CI -1.78 to 3.80 Kg], p = 0.48). None of the selected studies evaluated muscle strength. Endurance and combined training increase physical function criteria but do not improve muscle mass criteria on sarcopenia in NAFLD patients. These results must be interpreted with caution for the small number of patients included in the RCTs analyzed, the different characteristics of the ET carried out, the non-use of resistance training, which prevents assess its effect on sarcopenia despite the evidence that recommends it and does not assessment muscle strength criteria in RCT include. Future research should include muscle strength assessments and resistance training to evaluate the effects in this condition. Exercise training is beneficial for sarcopenia in NAFLD but is necessary more experimental evidence to define the best type of training that positively affects the three criteria of sarcopenia. PROSPERO reference number CRD42020191471.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.
Similar Articles
- Sandra Zampieri, Ines Bersch, Piera Smeriglio, Elena Barbieri, Massimo Ganassi, Christiaan Leeuwenburg, Riccardo Rosati, Paolo Gargiulo, Amber Pond, H. Lee Sweeney, Ugo Carraro, Five Padua days on muscle and mobility medicine (2024Pdm3) 27 February - 2 March, 2024 at Hotel Petrarca, Thermae of Euganean Hills, Padua, and San Luca Hall, Prato della Valle, Padua, Italy , European Journal of Translational Myology: Vol. 33 No. 4 (2023)
- Sandra Zampieri, Ines Bersch, Piera Smeriglio, Elena Barbieri, Simona Boncompagni, Maria Chiara Maccarone, Ugo Carraro, Program with last minute abstracts of the Padua Days on Muscle and Mobility Medicine, 27 February – 2 March, 2024 (2024Pdm3) , European Journal of Translational Myology: Vol. 34 No. 1 (2024)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejtm.2021.9630
https://doi.org/10.4081/ejtm.2021.9630



