Balance and muscle strength tests in patients with osteoporotic vertebral fractures to develop tailored rehabilitation programs
Accepted: 30 July 2020
HTML: 3
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
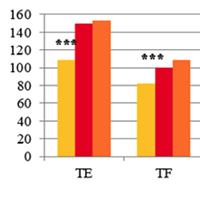
Authors perform a cross-sectional study of functional abilities of the patients with osteoporotic VF. Trunk muscle isometric strength and balance impairments were estimated. The development of osteoporotic VFs is associated with a significant decrease in strength of all the body muscles, especially the deep spinal stabilization system (TE, TF), where the VFs contribute to inappropriate distribution of back muscle strength with TE:TF ration of 1:1 instead of 3:2, observed both normally and in patients with uncomplicated osteoporosis. There is also a deterioration of stabilometry and functional balance assessment tests in patients with pathological VFs, which indicates abnormalities of both static and dynamic balance. The obtained data should be taken into account when developing rehabilitation programmes for patients with osteoporosis who have suffered compression VFs.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.
Similar Articles
- Nicola Manocchio, Isabella Iovene, Antonio Santoro, Maria Chiara Maccarone, Calogero Foti, Report and Abstracts of the 15th Congress of the Mediterranean Forum of Physical and Rehabilitation Medicine: Rome, July 6-8, 2023 , European Journal of Translational Myology: Vol. 33 No. 4 (2023)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejtm.2020.9236
https://doi.org/10.4081/ejtm.2020.9236



