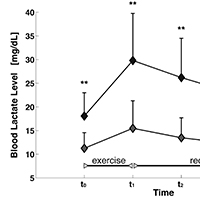
Muscle function impairment in cancer patients in pre-cachexia stage
Submitted: 28 February 2020
Accepted: 28 March 2020
Published: 22 June 2020
Accepted: 28 March 2020
Abstract Views: 894
PDF: 413
HTML: 33
HTML: 33
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Sandra Zampieri, Ines Bersch, Piera Smeriglio, Elena Barbieri, Simona Boncompagni, Maria Chiara Maccarone, Ugo Carraro, Program with last minute abstracts of the Padua Days on Muscle and Mobility Medicine, 27 February – 2 March, 2024 (2024Pdm3) , European Journal of Translational Myology: Vol. 34 No. 1 (2024)
- Sandra Zampieri, Ines Bersch, Piera Smeriglio, Elena Barbieri, Massimo Ganassi, Christiaan Leeuwenburg, Riccardo Rosati, Paolo Gargiulo, Amber Pond, H. Lee Sweeney, Ugo Carraro, Five Padua days on muscle and mobility medicine (2024Pdm3) 27 February - 2 March, 2024 at Hotel Petrarca, Thermae of Euganean Hills, Padua, and San Luca Hall, Prato della Valle, Padua, Italy , European Journal of Translational Myology: Vol. 33 No. 4 (2023)
- Francesca Riuzzi, Emanuele Mocciaro, Report and Abstracts of the 20th Meeting of IIM, the Interuniversity Institute of Myology: Assisi, October 12-15, 2023 , European Journal of Translational Myology: Vol. 34 No. 2 (2024)
- Maurilio Sampaolesi, Stefania Fulle, Report and Abstracts of the 19th Meeting of the Interuniversity Institute of Myology: Assisi, October 20-23, 2022 , European Journal of Translational Myology: Vol. 33 No. 2 (2023)
- The Editors, Abstracts of the XII Annual Meeting of the Interuniversity Institute of Myology | Reggio Emilia, Italy, October 1-4, 2015 , European Journal of Translational Myology: Vol. 26 No. 1 (2016)
- The Editors, Abstracts of the 2016 Spring Padua Muscle Days: Muscle decline in aging and neuromuscular disorders - Mechanisms and countermeasures | Terme Euganee, Padua, Italy, April 13-16, 2016 , European Journal of Translational Myology: Vol. 26 No. 1 (2016)
- Francesco Coscia, Ester Sara Di Filippo , Paola Virginia Gigliotti, Giorgio Fano Illic, Effect of physical activity on long COVID fatigue: an unsolved enigma , European Journal of Translational Myology: Vol. 33 No. 3 (2023)
- Paul Dowling, Stephen Gargan, Margit Zweyer, Michael Henry, Paula Meleady, Dieter Swandulla, Kay Ohlendieck, Proteomic reference map for sarcopenia research: mass spectrometric identification of key muscle proteins located in the sarcomere, cytoskeleton and the extracellular matrix , European Journal of Translational Myology: Vol. 34 No. 2 (2024)
- Paul Dowling, Stephen Gargan, Margit Zweyer, Michael Henry, Paula Meleady, Dieter Swandulla, Kay Ohlendieck, Proteomic reference map for sarcopenia research: mass spectrometric identification of key muscle proteins of organelles, cellular signaling, bioenergetic metabolism and molecular chaperoning , European Journal of Translational Myology: Vol. 34 No. 2 (2024)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejtm.2020.8931
https://doi.org/10.4081/ejtm.2020.8931



