Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Fibrin sealants in lumbar annuloplasty after endoscopic discectomy as a method to prevent recurrent lumbar disc herniation
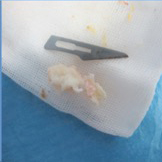
Fibrin sealant as a promising agent for providing scaffold and efficient hemostasis is widely accepted in several specialties. However, the outcome of Fibrin sealants in lumbar annuloplasty after endoscopic discectomy has not been evaluated in patients with disc herniation. The goal of this study was to evaluate the efficacy, response, and probability of future recurrence rates in herniated nucleus pulposus (HNP) with the use of fibrin sealant in conjunction with endoscopic disc surgery. A total of 35 patients (28 men, 7women) were evaluated, including 18 patients who underwent endoscopic discectomy alone and 17 patients that received fibrin sealant at the site of annulus tear and endoscopic discectomy. All patients were followed through both clinical and imaging methods for an average of 10.5 months. Primary outcome measure was defined as lumbar decompression approved by imaging and symptom alleviation after endoscopic spinal discectomy with Visual Analogue Scale (VAS) score ≤ 4 (cut-off point). Median size of annular tearing was significantly lower in the endoscopic discectomy group (median, 3) (minimum, 2; maximum, 5); however, the corresponding factor in the endoscopic discectomy plus fibrin sealant group was significantly larger (median, 6) (minimum, 5; maximum, 10), with P <0.001. Only one patient in the endoscopic discectomy group had an HNP recurrence during follow-up compared to two patients in the endoscopic discectomy plus fibrin sealant group. Due to the temporary effects of fibrin sealant in preventing disc herniation and the observed recurrence rate in both the case and control groups, the results of this study suggest a role of fibrin sealants combined with endoscopic discectomy to prevent early HNP recurrence rate.
Downloads
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2020.8748
https://doi.org/10.4081/ejtm.2020.8748