0
0
0
0
 Smart Citations
Smart Citations0
0
0
0
Citing PublicationsSupportingMentioningContrasting
See how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Cellular pathogenesis of Duchenne muscular dystrophy: progressive myofibre degeneration, chronic inflammation, reactive myofibrosis and satellite cell dysfunction
Downloads
Ganassi M, Zammit PS. Involvement of muscle satellite cell dysfunction in neuromuscular disorders: Expanding the portfolio of satellite cell-opathies. Eur J Transl Myol. 2022 Mar 18;32(1):10064. PMID: 35302338; PMCID: PMC8992676.
DOI: https://doi.org/10.4081/ejtm.2022.10064
Mauro A. Satellite cell of skeletal muscle fibers. J Biophys Biochem Cytol. 1961 Feb;9(2):493-5. PMID: 13768451; PMCID: PMC2225012.
DOI: https://doi.org/10.1083/jcb.9.2.493
Katz B. The terminations of the afferent nerve fibre in the muscle spindle of the frog. Philos Trans R Soc Lond (Biol) 1961;243:221–240.
DOI: https://doi.org/10.1098/rstb.1961.0001
Scharner J, Zammit PS. The muscle satellite cell at 50: the formative years. Skelet Muscle. 2011 Aug 17;1(1):28. doi: 10.1186/2044-5040-1-28. PMID: 21849021; PMCID: PMC3177780.
DOI: https://doi.org/10.1186/2044-5040-1-28
Yablonka-Reuveni Z. The skeletal muscle satellite cell: still young and fascinating at 50. J Histochem Cytochem. 2011 Dec;59(12):1041-59. PMID: 22147605; PMCID: PMC3283088.
DOI: https://doi.org/10.1369/0022155411426780
Morgan JE, Partridge TA. Muscle satellite cells. Int J Biochem Cell Biol. 2003 Aug;35(8):1151-6. PMID: 12757751.
DOI: https://doi.org/10.1016/S1357-2725(03)00042-6
Zammit PS, Partridge TA, Yablonka-Reuveni Z. The skeletal muscle satellite cell: the stem cell that came in from the cold. J Histochem Cytochem. 2006 Nov;54(11):1177-91. Epub 2006 Aug 9. PMID: 16899758.
DOI: https://doi.org/10.1369/jhc.6R6995.2006
Engquist EN, Zammit PS. The Satellite Cell at 60: The Foundation Years. J Neuromuscul Dis. 2021;8(s2):S183-S203. PMID: 34459412; PMCID: PMC8673500.
DOI: https://doi.org/10.3233/JND-210705
Murach KA, Fry CS, Dupont-Versteegden EE, McCarthy JJ, Peterson CA. Fusion and beyond: Satellite cell contributions to loading-induced skeletal muscle adaptation. FASEB J. 2021 Oct;35(10):e21893. PMID: 34480776; PMCID: PMC9293230.
DOI: https://doi.org/10.1096/fj.202101096R
Sousa-Victor P, García-Prat L, Muñoz-Cánoves P. Control of satellite cell function in muscle regeneration and its disruption in ageing. Nat Rev Mol Cell Biol. 2022 Mar;23(3):204-226. Epub 2021 Oct 18. PMID: 34663964.
DOI: https://doi.org/10.1038/s41580-021-00421-2
Pang KT, Loo LSW, Chia S, Ong FYT, Yu H, Walsh I. Insight into muscle stem cell regeneration and mechanobiology. Stem Cell Res Ther. 2023 May 12;14(1):129. PMID: 37173707; PMCID: PMC10176686.
DOI: https://doi.org/10.1186/s13287-023-03363-y
Mussini I, Favaro G, Carraro U. Maturation, dystrophic changes and the continuous production of fibers in skeletal muscle regenerating in the absence of nerve. J Neuropathol Exp Neurol. 1987 May;46(3):315-31. PMID: 3559631.
DOI: https://doi.org/10.1097/00005072-198705000-00007
Carraro U, Boncompagni S, Gobbo V, Rossini K, Zampieri S, Mosole S, Ravara B, Nori A, Stramare R, Ambrosio F, Piccione F, Masiero S, Vindigni V, Gargiulo P, Protasi F, Kern H, Pond A, Marcante A. Persistent Muscle Fiber Regeneration in Long Term Denervation. Past, Present, Future. Eur J Transl Myol. 2015 Mar 11;25(2):4832. PMID: 26913148; PMCID: PMC4383182.
DOI: https://doi.org/10.4081/bam.2015.2.77
Wang YX, Rudnicki MA. Satellite cells, the engines of muscle repair. Nat Rev Mol Cell Biol. 2011 Dec 21;13(2):127-33. PMID: 22186952.
DOI: https://doi.org/10.1038/nrm3265
Chang NC, Chevalier FP, Rudnicki MA. Satellite Cells in Muscular Dystrophy - Lost in Polarity. Trends Mol Med. 2016 Jun;22(6):479-496. Epub 2016 May 5. PMID: 27161598; PMCID: PMC4885782.
DOI: https://doi.org/10.1016/j.molmed.2016.04.002
Yablonka-Reuveni Z, Anderson JE. Satellite cells from dystrophic (mdx) mice display accelerated differentiation in primary cultures and in isolated myofibers. Dev Dyn. 2006 Jan;235(1):203-12. PMID: 16258933.
DOI: https://doi.org/10.1002/dvdy.20602
Dumont NA, Wang YX, von Maltzahn J, Pasut A, Bentzinger CF, Brun CE, Rudnicki MA. Dystrophin expression in muscle stem cells regulates their polarity and asymmetric division. Nat Med. 2015 Dec;21(12):1455-63. Epub 2015 Nov 16. PMID: 26569381; PMCID: PMC4839960.
DOI: https://doi.org/10.1038/nm.3990
Ribeiro AF Jr, Souza LS, Almeida CF, Ishiba R, Fernandes SA, Guerrieri DA, Santos ALF, Onofre-Oliveira PCG, Vainzof M. Muscle satellite cells and impaired late stage regeneration in different murine models for muscular dystrophies. Sci Rep. 2019 Aug 14;9(1):11842. PMID: 31413358; PMCID: PMC6694188.
DOI: https://doi.org/10.1038/s41598-019-48156-7
Barthélémy F, Santoso JW, Rabichow L, Jin R, Little I, Nelson SF, McCain ML, Miceli MC. Modeling Patient-Specific Muscular Dystrophy Phenotypes and Therapeutic Responses in Reprogrammed Myotubes Engineered on Micromolded Gelatin Hydrogels. Front Cell Dev Biol. 2022 Apr 6;10:830415. PMID: 35465312; PMCID: PMC9020228.
DOI: https://doi.org/10.3389/fcell.2022.830415
Rosenberg AS, Puig M, Nagaraju K, Hoffman EP, Villalta SA, Rao VA, Wakefield LM, Woodcock J. Immune-mediated pathology in Duchenne muscular dystrophy. Sci Transl Med. 2015 Aug 5;7(299):299rv4. PMID: 26246170; PMCID: PMC5951380.
DOI: https://doi.org/10.1126/scitranslmed.aaa7322
Ohlendieck K, Swandulla D. Molekulare Pathogenese der Fibrose bei Muskeldystrophie vom Typ Duchenne [Molecular pathogenesis of Duchenne muscular dystrophy-related fibrosis]. Pathologe. 2017 Feb;38(1):21-29. German. PMID: 28097378.
DOI: https://doi.org/10.1007/s00292-017-0265-1
Bez Batti Angulski A, Hosny N, Cohen H, Martin AA, Hahn D, Bauer J, Metzger JM. Duchenne muscular dystrophy: disease mechanism and therapeutic strategies. Front Physiol. 2023 Jun 26;14:1183101. PMID: 37435300; PMCID: PMC10330733.
DOI: https://doi.org/10.3389/fphys.2023.1183101
Duan D, Goemans N, Takeda S, Mercuri E, Aartsma-Rus A. Duchenne muscular dystrophy. Nat Rev Dis Primers. 2021 Feb 18;7(1):13. PMID: 33602943.
DOI: https://doi.org/10.1038/s41572-021-00248-3
Hoffman EP. The discovery of dystrophin, the protein product of the Duchenne muscular dystrophy gene. FEBS J. 2020 Sep;287(18):3879-3887. Epub 2020 Jul 21. PMID: 32608079; PMCID: PMC7540009.
DOI: https://doi.org/10.1111/febs.15466
Muntoni F, Torelli S, Ferlini A. Dystrophin and mutations: one gene, several proteins, multiple phenotypes. Lancet Neurol. 2003 Dec;2(12):731-40. PMID: 14636778.
DOI: https://doi.org/10.1016/S1474-4422(03)00585-4
Ferlini A, Neri M, Gualandi F. The medical genetics of dystrophinopathies: molecular genetic diagnosis and its impact on clinical practice. Neuromuscul Disord. 2013 Jan;23(1):4-14. Epub 2012 Oct 30. PMID: 23116935.
DOI: https://doi.org/10.1016/j.nmd.2012.09.002
Gaina G, Vossen RHAM, Manole E, Plesca DA, Ionica E. Combining Protein Expression and Molecular Data Improves Mutation Characterization of Dystrophinopathies. Front Neurol. 2021 Dec 7;12:718396. doi: 10.3389/fneur.2021.718396. PMID: 34950096; PMCID: PMC8689184.
DOI: https://doi.org/10.3389/fneur.2021.718396
Bello L, Hoffman EP, Pegoraro E. Is it time for genetic modifiers to predict prognosis in Duchenne muscular dystrophy? Nat Rev Neurol. 2023 Jul;19(7):410-423. Epub 2023 Jun 12. PMID: 37308617.
DOI: https://doi.org/10.1038/s41582-023-00823-0
Schultz TI, Raucci FJ Jr, Salloum FN. Cardiovascular Disease in Duchenne Muscular Dystrophy: Overview and Insight Into Novel Therapeutic Targets. JACC Basic Transl Sci. 2022 Mar 9;7(6):608-625. PMID: 35818510; PMCID: PMC9270569.
DOI: https://doi.org/10.1016/j.jacbts.2021.11.004
Pascual-Morena C, Cavero-Redondo I, Martínez-Vizcaíno V, Sequí-Domínguez I, Fernández-Bravo-Rodrigo J, Jiménez-López E. Dystrophin Genotype and Risk of Neuropsychiatric Disorders in Dystrophinopathies: A Systematic Review and Meta-Analysis. J Neuromuscul Dis. 2023;10(2):159-172. PMID: 36565132; PMCID: PMC10041431.
DOI: https://doi.org/10.3233/JND-221586
Ohlendieck K, Swandulla D. Complexity of skeletal muscle degeneration: multi-systems pathophysiology and organ crosstalk in dystrophinopathy. Pflugers Arch. 2021 Dec;473(12):1813-1839. Epub 2021 Sep 22. PMID: 34553265; PMCID: PMC8599371.
DOI: https://doi.org/10.1007/s00424-021-02623-1
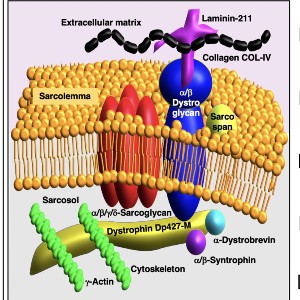
Murphy S, Ohlendieck K. The biochemical and mass spectrometric profiling of the dystrophin complexome from skeletal muscle. Comput Struct Biotechnol J. 2015 Nov 26;14:20-7. PMID: 26793286; PMCID: PMC4688399.
DOI: https://doi.org/10.1016/j.csbj.2015.11.002
Ohlendieck K. Towards an understanding of the dystrophin-glycoprotein complex: linkage between the extracellular matrix and the membrane cytoskeleton in muscle fibers. Eur J Cell Biol. 1996 Jan;69(1):1-10. PMID: 8825019.
Dowling P, Gargan S, Murphy S, Zweyer M, Sabir H, Swandulla D, Ohlendieck K. The Dystrophin Node as Integrator of Cytoskeletal Organization, Lateral Force Transmission, Fiber Stability and Cellular Signaling in Skeletal Muscle. Proteomes. 2021 Feb 2;9(1):9. PMID: 33540575; PMCID: PMC7931087.
DOI: https://doi.org/10.3390/proteomes9010009
Partridge TA. Impending therapies for Duchenne muscular dystrophy. Curr Opin Neurol. 2011 Oct;24(5):415-22. PMID: 21892079.
DOI: https://doi.org/10.1097/WCO.0b013e32834aa3f1
Chemello F, Olson EN, Bassel-Duby R. CRISPR-Editing Therapy for Duchenne Muscular Dystrophy. Hum Gene Ther. 2023 May;34(9-10):379-387. PMID: 37060194; PMCID: PMC10210224.
DOI: https://doi.org/10.1089/hum.2023.053
Mercuri E, Seferian AM, Servais L, Deconinck N, Stevenson H, Ni X, Zhang W, East L, Yonren S, Muntoni F; 4658-102 Study Group. Safety, tolerability and pharmacokinetics of eteplirsen in young boys aged 6-48 months with Duchenne muscular dystrophy amenable to exon 51 skipping. Neuromuscul Disord. 2023 Jun;33(6):476-483. Epub 2023 Mar 24. PMID: 37207382.
DOI: https://doi.org/10.1016/j.nmd.2023.03.008
Duan D. Duchenne Muscular Dystrophy Gene Therapy in 2023: Status, Perspective, and Beyond. Hum Gene Ther. 2023 May;34(9-10):345-349. PMID: 37219994; PMCID: PMC10325806.
DOI: https://doi.org/10.1089/hum.2023.29242.ddu
Dowling P, Murphy S, Zweyer M, Raucamp M, Swandulla D, Ohlendieck K. Emerging proteomic biomarkers of X-linked muscular dystrophy. Expert Rev Mol Diagn. 2019 Aug;19(8):739-755. Epub 2019 Aug 2. PMID: 31359811.
DOI: https://doi.org/10.1080/14737159.2019.1648214
Al-Khalili Szigyarto C. Duchenne Muscular Dystrophy: recent advances in protein biomarkers and the clinical application. Expert Rev Proteomics. 2020 May;17(5):365-375. PMID: 32713262.
DOI: https://doi.org/10.1080/14789450.2020.1773806
Fortunato F, Ferlini A. Biomarkers in Duchenne Muscular Dystrophy: Current Status and Future Directions. J Neuromuscul Dis. 2023 Jul 29. Epub ahead of print. PMID: 37545256.
DOI: https://doi.org/10.3233/JND-221666
Ervasti JM, Ohlendieck K, Kahl SD, Gaver MG, Campbell KP. Deficiency of a glycoprotein component of the dystrophin complex in dystrophic muscle. Nature. 1990 May 24;345(6273):315-9. PMID: 2188135.
DOI: https://doi.org/10.1038/345315a0
Ohlendieck K, Campbell KP. Dystrophin-associated proteins are greatly reduced in skeletal muscle from mdx mice. J Cell Biol. 1991 Dec;115(6):1685-94. PMID: 1757468; PMCID: PMC2289197.
DOI: https://doi.org/10.1083/jcb.115.6.1685
Ohlendieck K, Matsumura K, Ionasescu VV, Towbin JA, Bosch EP, Weinstein SL, Sernett SW, Campbell KP. Duchenne muscular dystrophy: deficiency of dystrophin-associated proteins in the sarcolemma. Neurology. 1993 Apr;43(4):795-800. PMID: 8469343.
DOI: https://doi.org/10.1212/WNL.43.4.795
Murphy S, Zweyer M, Henry M, Meleady P, Mundegar RR, Swandulla D, Ohlendieck K. Proteomic analysis of the sarcolemma-enriched fraction from dystrophic mdx-4cv skeletal muscle. J Proteomics. 2019 Jan 16;191:212-227. Epub 2018 Feb 2. PMID: 29408692.
DOI: https://doi.org/10.1016/j.jprot.2018.01.015
Zabłocka B, Górecki DC, Zabłocki K. Disrupted Calcium Homeostasis in Duchenne Muscular Dystrophy: A Common Mechanism behind Diverse Consequences. Int J Mol Sci. 2021 Oct 13;22(20):11040. PMID: 34681707; PMCID: PMC8537421.
DOI: https://doi.org/10.3390/ijms222011040
Culligan K, Banville N, Dowling P, Ohlendieck K. Drastic reduction of calsequestrin-like proteins and impaired calcium binding in dystrophic mdx muscle. J Appl Physiol (1985). 2002 Feb;92(2):435-45. PMID: 11796649.
DOI: https://doi.org/10.1152/japplphysiol.00903.2001
Dowling P, Doran P, Ohlendieck K. Drastic reduction of sarcalumenin in Dp427 (dystrophin of 427 kDa)-deficient fibres indicates that abnormal calcium handling plays a key role in muscular dystrophy. Biochem J. 2004 Apr 15;379(Pt 2):479-88. PMID: 14678011; PMCID: PMC1224066.
DOI: https://doi.org/10.1042/bj20031311
Dowling P, Gargan S, Swandulla D, Ohlendieck K. Proteomic profiling of impaired excitation-contraction coupling and abnormal calcium handling in muscular dystrophy. Proteomics. 2022 Dec;22(23-24):e2200003. Epub 2022 Aug 8. PMID: 35902360; PMCID: PMC10078611.
DOI: https://doi.org/10.1002/pmic.202200003
Partridge TA. The mdx mouse model as a surrogate for Duchenne muscular dystrophy. FEBS J. 2013 Sep;280(17):4177-86. Epub 2013 Apr 22. PMID: 23551987; PMCID: PMC4147949.
DOI: https://doi.org/10.1111/febs.12267
Cassano M, Berardi E, Crippa S, Toelen J, Barthelemy I, Micheletti R, Chuah M, Vandendriessche T, Debyser Z, Blot S, Sampaolesi M. Alteration of cardiac progenitor cell potency in GRMD dogs. Cell Transplant. 2012;21(9):1945-67. Epub 2012 Apr 10. PMID: 22513051.
DOI: https://doi.org/10.3727/096368912X638919
Echigoya Y, Trieu N, Duddy W, Moulton HM, Yin H, Partridge TA, Hoffman EP, Kornegay JN, Rohret FA, Rogers CS, Yokota T. A Dystrophin Exon-52 Deleted Miniature Pig Model of Duchenne Muscular Dystrophy and Evaluation of Exon Skipping. Int J Mol Sci. 2021 Dec 2;22(23):13065. PMID: 34884867; PMCID: PMC8657897.
DOI: https://doi.org/10.3390/ijms222313065
Wilson K, Faelan C, Patterson-Kane JC, Rudmann DG, Moore SA, Frank D, Charleston J, Tinsley J, Young GD, Milici AJ. Duchenne and Becker Muscular Dystrophies: A Review of Animal Models, Clinical End Points, and Biomarker Quantification. Toxicol Pathol. 2017 Oct;45(7):961-976. Epub 2017 Oct 3. PMID: 28974147; PMCID: PMC5788182.
DOI: https://doi.org/10.1177/0192623317734823
Grounds MD, Terrill JR, Al-Mshhdani BA, Duong MN, Radley-Crabb HG, Arthur PG. Biomarkers for Duchenne muscular dystrophy: myonecrosis, inflammation and oxidative stress. Dis Model Mech. 2020 Mar 2;13(2):dmm043638. PMID: 32224496; PMCID: PMC7063669.
DOI: https://doi.org/10.1242/dmm.043638
Mázala DAG, Hindupur R, Moon YJ, Shaikh F, Gamu IH, Alladi D, Panci G, Weiss-Gayet M, Chazaud B, Partridge TA, Novak JS, Jaiswal JK. Altered muscle niche contributes to myogenic deficit in the D2-mdx model of severe DMD. Cell Death Discov. 2023 Jul 4;9(1):224. PMID: 37402716; PMCID: PMC10319851.
DOI: https://doi.org/10.1038/s41420-023-01503-0
Mázala DA, Novak JS, Hogarth MW, Nearing M, Adusumalli P, Tully CB, Habib NF, Gordish-Dressman H, Chen YW, Jaiswal JK, Partridge TA. TGF-β-driven muscle degeneration and failed regeneration underlie disease onset in a DMD mouse model. JCI Insight. 2020 Mar 26;5(6):e135703. PMID: 32213706; PMCID: PMC7213798.
DOI: https://doi.org/10.1172/jci.insight.135703
Gargan S, Dowling P, Zweyer M, Henry M, Meleady P, Swandulla D, Ohlendieck K. Proteomic Identification of Markers of Membrane Repair, Regeneration and Fibrosis in the Aged and Dystrophic Diaphragm. Life (Basel). 2022 Oct 22;12(11):1679. PMID: 36362832; PMCID: PMC9696191.
DOI: https://doi.org/10.3390/life12111679
Zweyer M, Sabir H, Dowling P, Gargan S, Murphy S, Swandulla D, Ohlendieck K. Histopathology of Duchenne muscular dystrophy in correlation with changes in proteomic biomarkers. Histol Histopathol. 2022 Feb;37(2):101-116. Epub 2021 Dec 7. PMID: 34873679.
Starosta A, Konieczny P. Therapeutic aspects of cell signaling and communication in Duchenne muscular dystrophy. Cell Mol Life Sci. 2021 Jun;78(11):4867-4891. Epub 2021 Apr 7. PMID: 33825942; PMCID: PMC8233280.
DOI: https://doi.org/10.1007/s00018-021-03821-x
Tidball JG, Welc SS, Wehling-Henricks M. Immunobiology of Inherited Muscular Dystrophies. Compr Physiol. 2018 Sep 14;8(4):1313-1356. PMID: 30215857; PMCID: PMC7769418.
DOI: https://doi.org/10.1002/cphy.c170052
Bonomo AC, Pinto-Mariz F, Riederer I, Benjamim CF, Butler-Browne G, Mouly V, Savino W. Crosstalk Between Innate and T Cell Adaptive Immunity With(in) the Muscle. Front Physiol. 2020 Sep 18;11:573347. PMID: 33071827; PMCID: PMC7531250.
DOI: https://doi.org/10.3389/fphys.2020.573347
Spencer MJ, Montecino-Rodriguez E, Dorshkind K, Tidball JG. Helper (CD4(+)) and cytotoxic (CD8(+)) T cells promote the pathology of dystrophin-deficient muscle. Clin Immunol. 2001 Feb;98(2):235-43. PMID: 11161980.
DOI: https://doi.org/10.1006/clim.2000.4966
Mojumdar K, Liang F, Giordano C, Lemaire C, Danialou G, Okazaki T, Bourdon J, Rafei M, Galipeau J, Divangahi M, Petrof BJ. Inflammatory monocytes promote progression of Duchenne muscular dystrophy and can be therapeutically targeted via CCR2. EMBO Mol Med. 2014 Nov;6(11):1476-92. PMID: 25312642; PMCID: PMC4237472.
DOI: https://doi.org/10.15252/emmm.201403967
Dowling P, Gargan S, Zweyer M, Henry M, Meleady P, Swandulla D, Ohlendieck K. Proteome-wide Changes in the mdx-4cv Spleen due to Pathophysiological Cross Talk with Dystrophin-Deficient Skeletal Muscle. iScience. 2020 Aug 26;23(9):101500. Epub ahead of print. PMID: 32916630; PMCID: PMC7490529.
DOI: https://doi.org/10.1016/j.isci.2020.101500
Dowling P, Gargan S, Zweyer M, Henry M, Meleady P, Swandulla D, Ohlendieck K. Protocol for the Bottom-Up Proteomic Analysis of Mouse Spleen. STAR Protoc. 2020 Dec 3;1(3):100196. PMID: 33377090; PMCID: PMC7757555.
DOI: https://doi.org/10.1016/j.xpro.2020.100196
Rizzo G, Di Maggio R, Benedetti A, Morroni J, Bouche M, Lozanoska-Ochser B. Splenic Ly6Chi monocytes are critical players in dystrophic muscle injury and repair. JCI Insight. 2020 Jan 30;5(2):e130807. PMID: 31874104; PMCID: PMC7098719.
DOI: https://doi.org/10.1172/jci.insight.130807
Strizova Z, Benesova I, Bartolini R, Novysedlak R, Cecrdlova E, Foley LK, Striz I. M1/M2 macrophages and their overlaps - myth or reality? Clin Sci (Lond). 2023 Aug 14;137(15):1067-1093. PMID: 37530555; PMCID: PMC10407193.
DOI: https://doi.org/10.1042/CS20220531
Spencer MJ, Tidball JG. Do immune cells promote the pathology of dystrophin-deficient myopathies? Neuromuscul Disord. 2001 Sep;11(6-7):556-64. PMID: 11525885.
DOI: https://doi.org/10.1016/S0960-8966(01)00198-5
Malecova B, Gatto S, Etxaniz U, Passafaro M, Cortez A, Nicoletti C, Giordani L, Torcinaro A, De Bardi M, Bicciato S, De Santa F, Madaro L, Puri PL. Dynamics of cellular states of fibro-adipogenic progenitors during myogenesis and muscular dystrophy. Nat Commun. 2018 Sep 10;9(1):3670. PMID: 30202063; PMCID: PMC6131350.
DOI: https://doi.org/10.1038/s41467-018-06068-6
Negroni E, Kondili M, Muraine L, Bensalah M, Butler-Browne GS, Mouly V, Bigot A, Trollet C. Muscle fibro-adipogenic progenitors from a single-cell perspective: Focus on their "virtual" secretome. Front Cell Dev Biol. 2022 Sep 19;10:952041. PMID: 36200044; PMCID: PMC9527288.
DOI: https://doi.org/10.3389/fcell.2022.952041
Biferali B, Proietti D, Mozzetta C, Madaro L. Fibro-Adipogenic Progenitors Cross-Talk in Skeletal Muscle: The Social Network. Front Physiol. 2019 Aug 21;10:1074. PMID: 31496956; PMCID: PMC6713247.
DOI: https://doi.org/10.3389/fphys.2019.01074
Molina T, Fabre P, Dumont NA. Fibro-adipogenic progenitors in skeletal muscle homeostasis, regeneration and diseases. Open Biol. 2021 Dec;11(12):210110. Epub 2021 Dec 8. PMID: 34875199; PMCID: PMC8651418.
DOI: https://doi.org/10.1098/rsob.210110
Theret M, Rossi FMV, Contreras O. Evolving Roles of Muscle-Resident Fibro-Adipogenic Progenitors in Health, Regeneration, Neuromuscular Disorders, and Aging. Front Physiol. 2021 Apr 20;12:673404. doi: 10.3389/fphys.2021.673404. PMID: 33959042; PMCID: PMC8093402.
DOI: https://doi.org/10.3389/fphys.2021.673404
Mojumdar K, Giordano C, Lemaire C, Liang F, Divangahi M, Qureshi ST, Petrof BJ. Divergent impact of Toll-like receptor 2 deficiency on repair mechanisms in healthy muscle versus Duchenne muscular dystrophy. J Pathol. 2016 May;239(1):10-22. Epub 2016 Mar 16. PMID: 26800321.
DOI: https://doi.org/10.1002/path.4689
Bello L, Pegoraro E. The "Usual Suspects": Genes for Inflammation, Fibrosis, Regeneration, and Muscle Strength Modify Duchenne Muscular Dystrophy. J Clin Med. 2019 May 10;8(5):649. PMID: 31083420; PMCID: PMC6571893.
DOI: https://doi.org/10.3390/jcm8050649
Giuliani G, Rosina M, Reggio A. Signaling pathways regulating the fate of fibro/adipogenic progenitors (FAPs) in skeletal muscle regeneration and disease. FEBS J. 2022 Nov;289(21):6484-6517. Epub 2021 Jul 6. PMID: 34143565.
DOI: https://doi.org/10.1111/febs.16080
Desguerre I, Mayer M, Leturcq F, Barbet JP, Gherardi RK, Christov C. Endomysial fibrosis in Duchenne muscular dystrophy: a marker of poor outcome associated with macrophage alternative activation. J Neuropathol Exp Neurol. 2009 Jul;68(7):762-73. PMID: 19535995.
DOI: https://doi.org/10.1097/NEN.0b013e3181aa31c2
Klingler W, Jurkat-Rott K, Lehmann-Horn F, Schleip R. The role of fibrosis in Duchenne muscular dystrophy. Acta Myol. 2012 Dec;31(3):184-95. PMID: 23620650; PMCID: PMC3631802.
Dowling P, Gargan S, Zweyer M, Swandulla D, Ohlendieck K. Extracellular Matrix Proteomics: The mdx-4cv Mouse Diaphragm as a Surrogate for Studying Myofibrosis in Dystrophinopathy. Biomolecules. 2023 Jul 12;13(7):1108. PMID: 37509144; PMCID: PMC10377647.
DOI: https://doi.org/10.3390/biom13071108
Holland A, Dowling P, Meleady P, Henry M, Zweyer M, Mundegar RR, Swandulla D, Ohlendieck K. Label-free mass spectrometric analysis of the mdx-4cv diaphragm identifies the matricellular protein periostin as a potential factor involved in dystrophinopathy-related fibrosis. Proteomics. 2015 Jul;15(13):2318-31. Epub 2015 Apr 1. PMID: 25737063.
DOI: https://doi.org/10.1002/pmic.201400471
Muraine L, Bensalah M, Butler-Browne G, Bigot A, Trollet C, Mouly V, Negroni E. Update on anti-fibrotic pharmacotherapies in skeletal muscle disease. Curr Opin Pharmacol. 2023 Feb;68:102332. Epub 2022 Dec 23. PMID: 36566666.
DOI: https://doi.org/10.1016/j.coph.2022.102332
Camps J, Breuls N, Sifrim A, Giarratana N, Corvelyn M, Danti L, Grosemans H, Vanuytven S, Thiry I, Belicchi M, Meregalli M, Platko K, MacDonald ME, Austin RC, Gijsbers R, Cossu G, Torrente Y, Voet T, Sampaolesi M. Interstitial Cell Remodeling Promotes Aberrant Adipogenesis in Dystrophic Muscles. Cell Rep. 2020 May 5;31(5):107597. PMID: 32375047.
DOI: https://doi.org/10.1016/j.celrep.2020.107597
Veeger TTJ, van Zwet EW, Al Mohamad D, Naarding KJ, van de Velde NM, Hooijmans MT, Webb AG, Niks EH, de Groot JH, Kan HE. Muscle architecture is associated with muscle fat replacement in Duchenne and Becker muscular dystrophies. Muscle Nerve. 2021 Nov;64(5):576-584. Epub 2021 Aug 25. PMID: 34383334; PMCID: PMC9290788.
DOI: https://doi.org/10.1002/mus.27399
Huysmans L, De Wel B, Claeys KG, Maes F. Automated MRI quantification of volumetric per-muscle fat fractions in the proximal leg of patients with muscular dystrophies. Front Neurol. 2023 May 24;14:1200727. PMID: 37292137; PMCID: PMC10244517.
DOI: https://doi.org/10.3389/fneur.2023.1200727
Hooijmans MT, Niks EH, Burakiewicz J, Anastasopoulos C, van den Berg SI, van Zwet E, Webb AG, Verschuuren JJGM, Kan HE. Non-uniform muscle fat replacement along the proximodistal axis in Duchenne muscular dystrophy. Neuromuscul Disord. 2017 May;27(5):458-464. Epub 2017 Feb 21. PMID: 28302391.
DOI: https://doi.org/10.1016/j.nmd.2017.02.009
Morgan JE, Zammit PS. Direct effects of the pathogenic mutation on satellite cell function in muscular dystrophy. Exp Cell Res. 2010 Nov 1;316(18):3100-8. Epub 2010 May 28. PMID: 20546725.
DOI: https://doi.org/10.1016/j.yexcr.2010.05.014
Buckingham M, Relaix F. PAX3 and PAX7 as upstream regulators of myogenesis. Semin Cell Dev Biol. 2015 Aug;44:115-25. Epub 2015 Sep 28. PMID: 26424495.
DOI: https://doi.org/10.1016/j.semcdb.2015.09.017
Zammit PS. Function of the myogenic regulatory factors Myf5, MyoD, Myogenin and MRF4 in skeletal muscle, satellite cells and regenerative myogenesis. Semin Cell Dev Biol. 2017 Dec;72:19-32. Epub 2017 Nov 15. PMID: 29127046.
DOI: https://doi.org/10.1016/j.semcdb.2017.11.011
Ganassi M, Badodi S, Ortuste Quiroga HP, Zammit PS, Hinits Y, Hughes SM. Myogenin promotes myocyte fusion to balance fibre number and size. Nat Commun. 2018 Oct 12;9(1):4232. PMID: 30315160; PMCID: PMC6185967.
DOI: https://doi.org/10.1038/s41467-018-06583-6
Chang NC, Rudnicki MA. Satellite cells: the architects of skeletal muscle. Curr Top Dev Biol. 2014;107:161-81. PMID: 24439806.
Rudnicki MA, Le Grand F, McKinnell I, Kuang S. The molecular regulation of muscle stem cell function. Cold Spring Harb Symp Quant Biol. 2008;73:323-31. Epub 2009 Mar 27. PMID: 19329572.
DOI: https://doi.org/10.1101/sqb.2008.73.064
Ganassi M, Badodi S, Wanders K, Zammit PS, Hughes SM. Myogenin is an essential regulator of adult myofibre growth and muscle stem cell homeostasis. Elife. 2020 Oct 1;9:e60445. PMID: 33001028; PMCID: PMC7599067.
DOI: https://doi.org/10.7554/eLife.60445
Massenet J, Gardner E, Chazaud B, Dilworth FJ. Epigenetic regulation of satellite cell fate during skeletal muscle regeneration. Skelet Muscle. 2021 Jan 11;11(1):4. PMID: 33431060; PMCID: PMC7798257.
DOI: https://doi.org/10.1186/s13395-020-00259-w
Kodippili K, Rudnicki MA. Satellite cell contribution to disease pathology in Duchenne muscular dystrophy. Front Physiol. 2023 May 30;14:1180980. PMID: 37324396; PMCID: PMC10266354.
DOI: https://doi.org/10.3389/fphys.2023.1180980
Kahn RE, Dayanidhi S, Lacham-Kaplan O, Hawley JA. Molecular clocks, satellite cells, and skeletal muscle regeneration. Am J Physiol Cell Physiol. 2023 Jun 1;324(6):C1332-C1340. Epub 2023 May 15. PMID: 37184229.
DOI: https://doi.org/10.1152/ajpcell.00073.2023
Johnson AL, Kamal M, Parise G. The Role of Supporting Cell Populations in Satellite Cell Mediated Muscle Repair. Cells. 2023 Jul 30;12(15):1968. PMID: 37566047.
DOI: https://doi.org/10.3390/cells12151968
Yablonka-Reuveni Z, Lepper C. New Insight into a Classic Stem Cell: the Satellite Cell may Communicate with the Muscle Fiber via Extracellular Vesicles-A Perspective on "Fusion-Independent Satellite Cell Communication to Muscle Fibers During Load-Induced Hypertrophy". Function (Oxf). 2020 Sep 3;1(2):zqaa015. PMID: 35330641; PMCID: PMC8788824.
DOI: https://doi.org/10.1093/function/zqaa015
Rugowska A, Starosta A, Konieczny P. Epigenetic modifications in muscle regeneration and progression of Duchenne muscular dystrophy. Clin Epigenetics. 2021 Jan 19;13(1):13. PMID: 33468200; PMCID: PMC7814631.
DOI: https://doi.org/10.1186/s13148-021-01001-z
Heslop L, Morgan JE, Partridge TA. Evidence for a myogenic stem cell that is exhausted in dystrophic muscle. J Cell Sci. 2000 Jun;113 ( Pt 12):2299-308. PMID: 10825301.
DOI: https://doi.org/10.1242/jcs.113.12.2299
Wakayama Y, Schotland DL, Bonilla E, Orecchio E. Quantitative ultrastructural study of muscle satellite cells in Duchenne dystrophy. Neurology. 1979 Mar;29(3):401-7. PMID: 571989.
DOI: https://doi.org/10.1212/WNL.29.3.401
Ishimoto S, Goto I, Ohta M, Kuroiwa Y. A quantitative study of the muscle satellite cells in various neuromuscular disorders. J Neurol Sci. 1983 Dec;62(1-3):303-14. PMID: 6668477.
DOI: https://doi.org/10.1016/0022-510X(83)90207-1
Watkins SC, Cullen MJ. A quantitative comparison of satellite cell ultrastructure in Duchenne muscular dystrophy, polymyositis, and normal controls. Muscle Nerve. 1986 Oct;9(8):724-30. PMID: 3785283.
DOI: https://doi.org/10.1002/mus.880090808
Watkins SC, Cullen MJ. A quantitative study of myonuclear and satellite cell nuclear size in Duchenne's muscular dystrophy, polymyositis and normal human skeletal muscle. Anat Rec. 1988 Sep;222(1):6-11. PMID: 3189887.
DOI: https://doi.org/10.1002/ar.1092220103
Kottlors M, Kirschner J. Elevated satellite cell number in Duchenne muscular dystrophy. Cell Tissue Res. 2010 Jun;340(3):541-8. Epub 2010 May 15. PMID: 20467789.
DOI: https://doi.org/10.1007/s00441-010-0976-6
Bankolé LC, Feasson L, Ponsot E, Kadi F. Fibre type-specific satellite cell content in two models of muscle disease. Histopathology. 2013 Dec;63(6):826-32. Epub 2013 Sep 20. PMID: 24111647.
DOI: https://doi.org/10.1111/his.12231
Webster C, Blau HM. Accelerated age-related decline in replicative life-span of Duchenne muscular dystrophy myoblasts: implications for cell and gene therapy. Somat Cell Mol Genet. 1990 Nov;16(6):557-65. PMID: 2267630.
DOI: https://doi.org/10.1007/BF01233096
Boldrin L, Zammit PS, Morgan JE. Satellite cells from dystrophic muscle retain regenerative capacity. Stem Cell Res. 2015 Jan;14(1):20-9. Epub 2014 Nov 1. PMID: 25460248; PMCID: PMC4305370.
DOI: https://doi.org/10.1016/j.scr.2014.10.007
Matecki S, Guibinga GH, Petrof BJ. Regenerative capacity of the dystrophic (mdx) diaphragm after induced injury. Am J Physiol Regul Integr Comp Physiol. 2004 Oct;287(4):R961-8. Epub 2004 Jun 10. PMID: 15191902.
DOI: https://doi.org/10.1152/ajpregu.00146.2004
Jiang C, Wen Y, Kuroda K, Hannon K, Rudnicki MA, Kuang S. Notch signaling deficiency underlies age-dependent depletion of satellite cells in muscular dystrophy. Dis Model Mech. 2014 Aug;7(8):997-1004. Epub 2014 Jun 6. PMID: 24906372; PMCID: PMC4107328.
Lu A, Poddar M, Tang Y, Proto JD, Sohn J, Mu X, Oyster N, Wang B, Huard J. Rapid depletion of muscle progenitor cells in dystrophic mdx/utrophin-/- mice. Hum Mol Genet. 2014 Sep 15;23(18):4786-800. Epub 2014 Apr 29. PMID: 24781208; PMCID: PMC4140461.
DOI: https://doi.org/10.1093/hmg/ddu194
Zhang M, McLennan IS. Use of antibodies to identify satellite cells with a light microscope. Muscle Nerve. 1994 Sep;17(9):987-94. PMID: 8065401.
DOI: https://doi.org/10.1002/mus.880170905
Chang NC, Sincennes MC, Chevalier FP, Brun CE, Lacaria M, Segalés J, Muñoz-Cánoves P, Ming H, Rudnicki MA. The Dystrophin Glycoprotein Complex Regulates the Epigenetic Activation of Muscle Stem Cell Commitment. Cell Stem Cell. 2018 May 3;22(5):755-768.e6. Epub 2018 Apr 19. PMID: 29681515; PMCID: PMC5935555.
DOI: https://doi.org/10.1016/j.stem.2018.03.022
Gosselin MRF, Mournetas V, Borczyk M, Verma S, Occhipinti A, Róg J, Bozycki L, Korostynski M, Robson SC, Angione C, Pinset C, Gorecki DC. Loss of full-length dystrophin expression results in major cell-autonomous abnormalities in proliferating myoblasts. Elife. 2022 Sep 27;11:e75521. PMID: 36164827; PMCID: PMC9514850.
DOI: https://doi.org/10.7554/eLife.75521
Mournetas V, Massouridès E, Dupont JB, Kornobis E, Polvèche H, Jarrige M, Dorval ARL, Gosselin MRF, Manousopoulou A, Garbis SD, Górecki DC, Pinset C. Myogenesis modelled by human pluripotent stem cells: a multi-omic study of Duchenne myopathy early onset. J Cachexia Sarcopenia Muscle. 2021 Feb;12(1):209-232. Epub 2021 Feb 14. PMID: 33586340; PMCID: PMC7890274.
DOI: https://doi.org/10.1002/jcsm.12665
Róg J, Oksiejuk A, Gosselin MRF, Brutkowski W, Dymkowska D, Nowak N, Robson S, Górecki DC, Zabłocki K. Dystrophic mdx mouse myoblasts exhibit elevated ATP/UTP-evoked metabotropic purinergic responses and alterations in calcium signalling. Biochim Biophys Acta Mol Basis Dis. 2019 Jun 1;1865(6):1138-1151. Epub 2019 Jan 24. PMID: 30684640.
DOI: https://doi.org/10.1016/j.bbadis.2019.01.002
Róg J, Oksiejuk A, Górecki DC, Zabłocki K. Primary mouse myoblast metabotropic purinoceptor profiles and calcium signalling differ with their muscle origin and are altered in mdx dystrophinopathy. Sci Rep. 2023 Jun 8;13(1):9333. PMID: 37291185; PMCID: PMC10250391.
DOI: https://doi.org/10.1038/s41598-023-36545-y
Shoji E, Sakurai H, Nishino T, Nakahata T, Heike T, Awaya T, Fujii N, Manabe Y, Matsuo M, Sehara-Fujisawa A. Early pathogenesis of Duchenne muscular dystrophy modelled in patient-derived human induced pluripotent stem cells. Sci Rep. 2015 Aug 20;5:12831. PMID: 26290039; PMCID: PMC4642533.
DOI: https://doi.org/10.1038/srep12831
Yoshioka K, Ito A, Horie M, Ikeda K, Kataoka S, Sato K, Yoshigai T, Sakurai H, Hotta A, Kawabe Y, Kamihira M. Contractile Activity of Myotubes Derived from Human Induced Pluripotent Stem Cells: A Model of Duchenne Muscular Dystrophy. Cells. 2021 Sep 27;10(10):2556. PMID: 34685536; PMCID: PMC8534131.
DOI: https://doi.org/10.3390/cells10102556
Onopiuk M, Brutkowski W, Wierzbicka K, Wojciechowska S, Szczepanowska J, Fronk J, Lochmüller H, Górecki DC, Zabłocki K. Mutation in dystrophin-encoding gene affects energy metabolism in mouse myoblasts. Biochem Biophys Res Commun. 2009 Aug 28;386(3):463-6. Epub 2009 Jun 13. PMID: 19527684.
DOI: https://doi.org/10.1016/j.bbrc.2009.06.053
Pant M, Sopariwala DH, Bal NC, Lowe J, Delfín DA, Rafael-Fortney J, Periasamy M. Metabolic dysfunction and altered mitochondrial dynamics in the utrophin-dystrophin deficient mouse model of duchenne muscular dystrophy. PLoS One. 2015 Apr 10;10(4):e0123875. PMID: 25859846; PMCID: PMC4393257.
DOI: https://doi.org/10.1371/journal.pone.0123875
Matre PR, Mu X, Wu J, Danila D, Hall MA, Kolonin MG, Darabi R, Huard J. CRISPR/Cas9-Based Dystrophin Restoration Reveals a Novel Role for Dystrophin in Bioenergetics and Stress Resistance of Muscle Progenitors. Stem Cells. 2019 Dec;37(12):1615-1628. Epub 2019 Nov 18. PMID: 31574188; PMCID: PMC6916636.
DOI: https://doi.org/10.1002/stem.3094
Sugihara H, Teramoto N, Nakamura K, Shiga T, Shirakawa T, Matsuo M, Ogasawara M, Nishino I, Matsuwaki T, Nishihara M, Yamanouchi K. Cellular senescence-mediated exacerbation of Duchenne muscular dystrophy. Sci Rep. 2020 Oct 12;10(1):16385. PMID: 33046751; PMCID: PMC7550355.
DOI: https://doi.org/10.1038/s41598-020-73315-6
Morgan J, Partridge T. Skeletal muscle in health and disease. Dis Model Mech. 2020 Feb 6;13(2):dmm042192. PMID: 32066552; PMCID: PMC7044447.
DOI: https://doi.org/10.1242/dmm.042192
Partridge TA. Enhancing Interrogation of Skeletal Muscle Samples for Informative Quantitative Data. J Neuromuscul Dis. 2021;8(s2):S257-S269. PMID: 34511511; PMCID: PMC8673506.
DOI: https://doi.org/10.3233/JND-210736
Gioftsidi S, Relaix F, Mourikis P. The Notch signaling network in muscle stem cells during development, homeostasis, and disease. Skelet Muscle. 2022 Apr 22;12(1):9. PMID: 35459219; PMCID: PMC9027478.
DOI: https://doi.org/10.1186/s13395-022-00293-w
Ohlendieck K, Ervasti JM, Snook JB, Campbell KP. Dystrophin-glycoprotein complex is highly enriched in isolated skeletal muscle sarcolemma. J Cell Biol. 1991 Jan;112(1):135-48. PMID: 1986002; PMCID: PMC2288808.
DOI: https://doi.org/10.1083/jcb.112.1.135
Ganassi M, Muntoni F, Zammit PS. Defining and identifying satellite cell-opathies within muscular dystrophies and myopathies. Exp Cell Res. 2022;411(1):112906. Epub 2021/11/07.
DOI: https://doi.org/10.1016/j.yexcr.2021.112906
McLoon LK, Wirtschafter J. Activated satellite cells in extraocular muscles of normal adult monkeys and humans. Invest Ophthalmol Vis Sci. 2003 May;44(5):1927-32. PMID: 12714625; PMCID: PMC1796845.
DOI: https://doi.org/10.1167/iovs.02-0673
Andrade FH, Porter JD, Kaminski HJ. Eye muscle sparing by the muscular dystrophies: lessons to be learned? Microsc Res Tech. 2000 Feb 1-15;48(3-4):192-203. PMID: 10679966.
DOI: https://doi.org/10.1002/(SICI)1097-0029(20000201/15)48:3/4<192::AID-JEMT7>3.0.CO;2-J
McDonald AA, Kunz MD, McLoon LK. Dystrophic changes in extraocular muscles after gamma irradiation in mdx:utrophin(+/-) mice. PLoS One. 2014 Jan 21;9(1):e86424. PMID: 24466085; PMCID: PMC3897728.
DOI: https://doi.org/10.1371/journal.pone.0086424
Stuelsatz P, Shearer A, Li Y, Muir LA, Ieronimakis N, Shen QW, Kirillova I, Yablonka-Reuveni Z. Extraocular muscle satellite cells are high performance myo-engines retaining efficient regenerative capacity in dystrophin deficiency. Dev Biol. 2015 Jan 1;397(1):31-44. Epub 2014 Sep 16. PMID: 25236433; PMCID: PMC4309674.
DOI: https://doi.org/10.1016/j.ydbio.2014.08.035
Formicola L, Marazzi G, Sassoon DA. The extraocular muscle stem cell niche is resistant to ageing and disease. Front Aging Neurosci. 2014 Dec 1;6:328. PMID: 25520657; PMCID: PMC4249457.
DOI: https://doi.org/10.3389/fnagi.2014.00328
Verma M, Fitzpatrick K, McLoon LK. Extraocular Muscle Repair and Regeneration. Curr Ophthalmol Rep. 2017 Sep;5(3):207-215. Epub 2017 Jun 16. PMID: 29109908; PMCID: PMC5669281.
DOI: https://doi.org/10.1007/s40135-017-0141-4
Hernandez-Torres F, Rodríguez-Outeiriño L, Franco D, Aranega AE. Pitx2 in Embryonic and Adult Myogenesis. Front Cell Dev Biol. 2017 May 1;5:46. PMID: 28507987; PMCID: PMC5410577.
DOI: https://doi.org/10.3389/fcell.2017.00046
Lewis C, Ohlendieck K. Proteomic profiling of naturally protected extraocular muscles from the dystrophin-deficient mdx mouse. Biochem Biophys Res Commun. 2010 Jun 11;396(4):1024-9. Epub 2010 May 22. PMID: 20471957.
DOI: https://doi.org/10.1016/j.bbrc.2010.05.052
Matsumura CY, Menezes de Oliveira B, Durbeej M, Marques MJ. Isobaric Tagging-Based Quantification for Proteomic Analysis: A Comparative Study of Spared and Affected Muscles from mdx Mice at the Early Phase of Dystrophy. PLoS One. 2013 Jun 18;8(6):e65831. PMID: 23823696; PMCID: PMC3688818.
DOI: https://doi.org/10.1371/journal.pone.0065831
Gargan S, Dowling P, Zweyer M, Reimann J, Henry M, Meleady P, Swandulla D, Ohlendieck K. Mass Spectrometric Profiling of Extraocular Muscle and Proteomic Adaptations in the mdx-4cv Model of Duchenne Muscular Dystrophy. Life (Basel). 2021 Jun 22;11(7):595. PMID: 34206383; PMCID: PMC8304255.
DOI: https://doi.org/10.3390/life11070595
Dowling P, Culligan K, Ohlendieck K. Distal mdx muscle groups exhibiting up-regulation of utrophin and rescue of dystrophin-associated glycoproteins exemplify a protected phenotype in muscular dystrophy. Naturwissenschaften. 2002 Feb;89(2):75-8. PMID: 12046625.
DOI: https://doi.org/10.1007/s00114-001-0289-4
Dowling P, Lohan J, Ohlendieck K. Comparative analysis of Dp427-deficient mdx tissues shows that the milder dystrophic phenotype of extraocular and toe muscle fibres is associated with a persistent expression of beta-dystroglycan. Eur J Cell Biol. 2003 May;82(5):222-30. PMID: 12800977.
DOI: https://doi.org/10.1078/0171-9335-00315
Ohlendieck K, Ervasti JM, Matsumura K, Kahl SD, Leveille CJ, Campbell KP. Dystrophin-related protein is localized to neuromuscular junctions of adult skeletal muscle. Neuron. 1991 Sep;7(3):499-508. PMID: 1654951.
DOI: https://doi.org/10.1016/0896-6273(91)90301-F
Zeiger U, Mitchell CH, Khurana TS. Superior calcium homeostasis of extraocular muscles. Exp Eye Res. 2010 Nov;91(5):613-22. Epub 2010 Aug 7. PMID: 20696159; PMCID: PMC4086352.
DOI: https://doi.org/10.1016/j.exer.2010.07.019
Zhang H, Liu Y, Li C, Zhang W. ITGβ6 Facilitates Skeletal Muscle Development by Maintaining the Properties and Cytoskeleton Stability of Satellite Cells. Life (Basel). 2022 Jun 21;12(7):926. PMID: 35888016; PMCID: PMC9318838.
DOI: https://doi.org/10.3390/life12070926
Chen M, Zhang L, Guo Y, Liu X, Song Y, Li X, Ding X, Guo H. A novel lncRNA promotes myogenesis of bovine skeletal muscle satellite cells via PFN1-RhoA/Rac1. J Cell Mol Med. 2021 May 4;25(13):5988–6005. Epub ahead of print. PMID: 33942976; PMCID: PMC8256363.
DOI: https://doi.org/10.1111/jcmm.16427
Baraibar M, Hyzewicz J, Rogowska-Wrzesinska A, Bulteau AL, Prip-Buus C, Butler-Browne G, Friguet B. Impaired metabolism of senescent muscle satellite cells is associated with oxidative modifications of glycolytic enzymes. Free Radic Biol Med. 2014 Oct;75 Suppl 1:S23. Epub 2014 Dec 10. PMID: 26461311.
DOI: https://doi.org/10.1016/j.freeradbiomed.2014.10.738
Beauchamp JR, Heslop L, Yu DS, Tajbakhsh S, Kelly RG, Wernig A, Buckingham ME, Partridge TA, Zammit PS. Expression of CD34 and Myf5 defines the majority of quiescent adult skeletal muscle satellite cells. J Cell Biol. 2000 Dec 11;151(6):1221-34. PMID: 11121437; PMCID: PMC2190588.
DOI: https://doi.org/10.1083/jcb.151.6.1221
Jankowski RJ, Deasy BM, Cao B, Gates C, Huard J. The role of CD34 expression and cellular fusion in the regeneration capacity of myogenic progenitor cells. J Cell Sci. 2002 Nov 15;115(Pt 22):4361-74. PMID: 12376567.
DOI: https://doi.org/10.1242/jcs.00110
Fernández-Lázaro D, Garrosa E, Seco-Calvo J, Garrosa M. Potential Satellite Cell-Linked Biomarkers in Aging Skeletal Muscle Tissue: Proteomics and Proteogenomics to Monitor Sarcopenia. Proteomes. 2022 Aug 19;10(3):29. PMID: 35997441; PMCID: PMC9396989.
DOI: https://doi.org/10.3390/proteomes10030029
Mansuri MS, Williams K, Nairn AC. Uncovering biology by single-cell proteomics. Commun Biol. 2023 Apr 8;6(1):381. PMID: 37031277; PMCID: PMC10082756.
DOI: https://doi.org/10.1038/s42003-023-04635-2
Ahmad R, Budnik B. A review of the current state of single-cell proteomics and future perspective. Anal Bioanal Chem. 2023 Jun 7. Epub ahead of print. PMID: 37285026.
DOI: https://doi.org/10.1007/s00216-023-04759-8
Slavov N. Scaling Up Single-Cell Proteomics. Mol Cell Proteomics. 2022 Jan;21(1):100179. Epub 2021 Nov 20. PMID: 34808355; PMCID: PMC8683604.
DOI: https://doi.org/10.1016/j.mcpro.2021.100179
Petrosius V, Schoof EM. Recent advances in the field of single-cell proteomics. Transl Oncol. 2023 Jan;27:101556. Epub 2022 Oct 19. PMID: 36270102; PMCID: PMC9587008.
DOI: https://doi.org/10.1016/j.tranon.2022.101556
Kim S, Kamarulzaman L, Taniguchi Y. Recent methodological advances towards single-cell proteomics. Proc Jpn Acad Ser B Phys Biol Sci. 2023 Sep 6. Epub ahead of print. PMID: 37673661.
Rosenberger FA, Thielert M, Mann M. Making single-cell proteomics biologically relevant. Nat Methods. 2023 Mar;20(3):320-323. PMID: 36899157.
DOI: https://doi.org/10.1038/s41592-023-01771-9
Wang Y, Lih TM, Chen L, Xu Y, Kuczler MD, Cao L, Pienta KJ, Amend SR, Zhang H. Optimized data-independent acquisition approach for proteomic analysis at single-cell level. Clin Proteomics. 2022 Jul 9;19(1):24. PMID: 35810282; PMCID: PMC9270744.
DOI: https://doi.org/10.1186/s12014-022-09359-9
Mun DG, Bhat FA, Ding H, Madden BJ, Natesampillai S, Badley AD, Johnson KL, Kelly RT, Pandey A. Optimizing single cell proteomics using trapped ion mobility spectrometry for label-free experiments. Analyst. 2023 Jul 26;148(15):3466-3475. PMID: 37395315; PMCID: PMC10370902.
DOI: https://doi.org/10.1039/D3AN00080J
Cong Y, Motamedchaboki K, Misal SA, Liang Y, Guise AJ, Truong T, Huguet R, Plowey ED, Zhu Y, Lopez-Ferrer D, Kelly RT. Ultrasensitive single-cell proteomics workflow identifies >1000 protein groups per mammalian cell. Chem Sci. 2020 Nov 17;12(3):1001-1006. PMID: 34163866; PMCID: PMC8178986.
DOI: https://doi.org/10.1039/D0SC03636F
Murgia M, Nogara L, Baraldo M, Reggiani C, Mann M, Schiaffino S. Protein profile of fiber types in human skeletal muscle: a single-fiber proteomics study. Skelet Muscle. 2021 Nov 2;11(1):24.. PMID: 34727990; PMCID: PMC8561870.
DOI: https://doi.org/10.1186/s13395-021-00279-0
Murgia M, Ciciliot S, Nagaraj N, Reggiani C, Schiaffino S, Franchi MV, Pišot R, Šimunič B, Toniolo L, Blaauw B, Sandri M, Biolo G, Flück M, Narici MV, Mann M. Signatures of muscle disuse in spaceflight and bed rest revealed by single muscle fiber proteomics. PNAS Nexus. 2022 Jun 11;1(3):pgac086. PMID: 36741463; PMCID: PMC9896895.
DOI: https://doi.org/10.1093/pnasnexus/pgac086
Schiaffino S, Reggiani C, Murgia M. Fiber type diversity in skeletal muscle explored by mass spectrometry-based single fiber proteomics. Histol Histopathol. 2020 Mar;35(3):239-246. Epub 2019 Oct 15. PMID: 31612964.
Momenzadeh A, Jiang Y, Kreimer S, Teigen LE, Zepeda CS, Haghani A, Mastali M, Song Y, Hutton A, Parker SJ, Van Eyk JE, Sundberg CW, Meyer JG. A Complete Workflow for High Throughput Human Single Skeletal Muscle Fiber Proteomics. J Am Soc Mass Spectrom. 2023 Sep 6;34(9):1858-1867. Epub 2023 Jul 18. PMID: 37463334.
DOI: https://doi.org/10.1021/jasms.3c00072
Borok M, Didier N, Gattazzo F, Ozturk T, Corneau A, Rouard H, Relaix F. Progressive and Coordinated Mobilization of the Skeletal Muscle Niche throughout Tissue Repair Revealed by Single-Cell Proteomic Analysis. Cells. 2021 Mar 28;10(4):744. PMID: 33800595; PMCID: PMC8066646.
DOI: https://doi.org/10.3390/cells10040744
Fabre P, Molina T, Orfi Z, Dumont NA. Assessment of Muscle Function Following hiPSC-Derived Myoblast Transplantation in Dystrophic Mice. Curr Protoc. 2022 Jan;2(1):e356. Erratum in: Curr Protoc. 2022 Aug;2(8):e554. PMID: 35085428.
DOI: https://doi.org/10.1002/cpz1.356
Fortunato F, Farnè M, Ferlini A. The DMD gene and therapeutic approaches to restore dystrophin. Neuromuscul Disord. 2021 Oct;31(10):1013-1020. PMID: 34736624.
DOI: https://doi.org/10.1016/j.nmd.2021.08.004
Fortunato F, Rossi R, Falzarano MS, Ferlini A. Innovative Therapeutic Approaches for Duchenne Muscular Dystrophy. J Clin Med. 2021 Feb 17;10(4):820. PMID: 33671409; PMCID: PMC7922390.
DOI: https://doi.org/10.3390/jcm10040820
Górecki DC. Dystrophin immunogenicity and requirement in myogenic cells: Paradigm shift in gene therapy for DMD. Clin Transl Med. 2022 Nov;12(11):e1122. PMID: 36424805; PMCID: PMC9691905.
DOI: https://doi.org/10.1002/ctm2.1122
Saleh KK, Switzler C, Hicks MR, Gane L, Gibbs DE, Pyle AD. Duchenne muscular dystrophy disease severity impacts skeletal muscle progenitor cells systemic delivery. Front Physiol. 2023 May 9;14:1190524. PMID: 37228827; PMCID: PMC10203213.
DOI: https://doi.org/10.3389/fphys.2023.1190524
Partridge TA, Morgan JE. Multiple insights from myogenic cell transplants. Hum Gene Ther. 2014 May;25(5):404-5. PMID: 24848316.
DOI: https://doi.org/10.1089/hum.2014.035
Dumont NA, Rudnicki MA. Targeting muscle stem cell intrinsic defects to treat Duchenne muscular dystrophy. NPJ Regen Med. 2016;1:16006–.Epub 2016 Jun 9. PMID: 29188075; PMCID: PMC5703417.
DOI: https://doi.org/10.1038/npjregenmed.2016.6
Filippelli RL, Chang NC. Empowering Muscle Stem Cells for the Treatment of Duchenne Muscular Dystrophy. Cells Tissues Organs. 2022;211(6):641-654. Epub 2021 Apr 28. PMID: 33910206.
DOI: https://doi.org/10.1159/000514305
Boyer O, Butler-Browne G, Chinoy H, Cossu G, Galli F, Lilleker JB, Magli A, Mouly V, Perlingeiro RCR, Previtali SC, Sampaolesi M, Smeets H, Schoewel-Wolf V, Spuler S, Torrente Y, Van Tienen F; Study Group. Myogenic Cell Transplantation in Genetic and Acquired Diseases of Skeletal Muscle. Front Genet. 2021 Aug 2;12:702547. PMID: 34408774; PMCID: PMC8365145.
DOI: https://doi.org/10.3389/fgene.2021.702547
Galli F, Mouly V, Butler-Browne G, Cossu G. Challenges in cell transplantation for muscular dystrophy. Exp Cell Res. 2021 Dec 1;409(1):112908. Epub 2021 Nov 1. PMID: 34736920.
DOI: https://doi.org/10.1016/j.yexcr.2021.112908
Sun C, Serra C, Lee G, Wagner KR. Stem cell-based therapies for Duchenne muscular dystrophy. Exp Neurol. 2020 Jan;323:113086. Epub 2019 Oct 19. PMID: 31639376; PMCID: PMC6899334.
DOI: https://doi.org/10.1016/j.expneurol.2019.113086
Ausems CRM, van Engelen BGM, van Bokhoven H, Wansink DG. Systemic cell therapy for muscular dystrophies : The ultimate transplantable muscle progenitor cell and current challenges for clinical efficacy. Stem Cell Rev Rep. 2021 Jun;17(3):878-899. Epub 2020 Dec 21. PMID: 33349909; PMCID: PMC8166694.
DOI: https://doi.org/10.1007/s12015-020-10100-y
Vallejo D, Hernández-Torres F, Lozano-Velasco E, Rodriguez-Outeiriño L, Carvajal A, Creus C, Franco D, Aránega AE. PITX2 Enhances the Regenerative Potential of Dystrophic Skeletal Muscle Stem Cells. Stem Cell Reports. 2018 Apr 10;10(4):1398-1411. PMID: 29641992; PMCID: PMC5998647.
DOI: https://doi.org/10.1016/j.stemcr.2018.03.009
McDonald CM, Henricson EK, Abresch RT, Duong T, Joyce NC, Hu F, Clemens PR, Hoffman EP, Cnaan A, Gordish-Dressman H; CINRG Investigators. Long-term effects of glucocorticoids on function, quality of life, and survival in patients with Duchenne muscular dystrophy: a prospective cohort study. Lancet. 2018 Feb 3;391(10119):451-461. Epub 2017 Nov 22. PMID: 29174484.
Merlini L, Cecconi I, Parmeggiani A, Cordelli DM, Dormi A. Quadriceps muscle strength in Duchenne muscular dystrophy and effect of corticosteroid treatment. Acta Myol. 2020 Dec 1;39(4):200-206. PMID: 33458575; PMCID: PMC7783426.
Hoffman EP. Pharmacotherapy of Duchenne Muscular Dystrophy. Handb Exp Pharmacol. 2020;261:25-37. PMID: 31375923.
DOI: https://doi.org/10.1007/164_2019_256
Grages SM, Bell M, Berlau DJ. New and emerging pharmacotherapy for duchenne muscular dystrophy: a focus on synthetic therapeutics. Expert Opin Pharmacother. 2020 May;21(7):841-851. Epub 2020 Mar 5. PMID: 32133879.
DOI: https://doi.org/10.1080/14656566.2020.1732350
Kawamura K, Fukumura S, Nikaido K, Tachi N, Kozuka N, Seino T, Hatakeyama K, Mori M, Ito YM, Takami A, Hinotsu S, Kuno A, Kawasaki Y, Horio Y, Tsutsumi H. Resveratrol improves motor function in patients with muscular dystrophies: an open-label, single-arm, phase IIa study. Sci Rep. 2020 Nov 25;10(1):20585. PMID: 33239684; PMCID: PMC7688653.
DOI: https://doi.org/10.1038/s41598-020-77197-6
Amor F, Vu Hong A, Corre G, Sanson M, Suel L, Blaie S, Servais L, Voit T, Richard I, Israeli D. Cholesterol metabolism is a potential therapeutic target in Duchenne muscular dystrophy. J Cachexia Sarcopenia Muscle. 2021 Jun;12(3):677-693. Epub 2021 May 26. PMID: 34037326; PMCID: PMC8200436.
DOI: https://doi.org/10.1002/jcsm.12708
Ziemba M, Barkhouse M, Uaesoontrachoon K, Giri M, Hathout Y, Dang UJ, Gordish-Dressman H, Nagaraju K, Hoffman EP. Biomarker-focused multi-drug combination therapy and repurposing trial in mdx mice. PLoS One. 2021 Feb 22;16(2):e0246507. PMID: 33617542; PMCID: PMC7899329.
DOI: https://doi.org/10.1371/journal.pone.0246507
Doran P, Wilton SD, Fletcher S, Ohlendieck K. Proteomic profiling of antisense-induced exon skipping reveals reversal of pathobiochemical abnormalities in dystrophic mdx diaphragm. Proteomics. 2009 Feb;9(3):671-85. PMID: 19132684; PMCID: PMC2770591.
DOI: https://doi.org/10.1002/pmic.200800441
Li D, Mastaglia FL, Fletcher S, Wilton SD. Precision Medicine through Antisense Oligonucleotide-Mediated Exon Skipping. Trends Pharmacol Sci. 2018 Nov;39(11):982-994. Epub 2018 Sep 30. PMID: 30282590.
DOI: https://doi.org/10.1016/j.tips.2018.09.001
Clemens PR, Rao VK, Connolly AM, Harper AD, Mah JK, Smith EC, McDonald CM, Zaidman CM, Morgenroth LP, Osaki H, Satou Y, Yamashita T, Hoffman EP; CINRG DNHS Investigators. Safety, Tolerability, and Efficacy of Viltolarsen in Boys With Duchenne Muscular Dystrophy Amenable to Exon 53 Skipping: A Phase 2 Randomized Clinical Trial. JAMA Neurol. 2020 Aug 1;77(8):982-991. Erratum in: JAMA Neurol. 2020 Aug 1;77(8):1040. PMID: 32453377; PMCID: PMC7251505.
DOI: https://doi.org/10.1001/jamaneurol.2020.1264
Novak JS, Spathis R, Dang UJ, Fiorillo AA, Hindupur R, Tully CB, Mázala DAG, Canessa E, Brown KJ, Partridge TA, Hathout Y, Nagaraju K. Interrogation of Dystrophin and Dystroglycan Complex Protein Turnover After Exon Skipping Therapy. J Neuromuscul Dis. 2021;8(s2):S383-S402. PMID: 34569969; PMCID: PMC8673539.
DOI: https://doi.org/10.3233/JND-210696
Vila MC, Novak JS, Benny Klimek M, Li N, Morales M, Fritz AG, Edwards K, Boehler JF, Hogarth MW, Kinder TB, Zhang A, Mazala D, Fiorillo AA, Douglas B, Chen YW, van den Anker J, Lu QL, Hathout Y, Hoffman EP, Partridge TA, Nagaraju K. Morpholino-induced exon skipping stimulates cell-mediated and humoral responses to dystrophin in mdx mice. J Pathol. 2019 Jul;248(3):339-351. Epub 2019 Apr 16. PMID: 30883742; PMCID: PMC6579705.
DOI: https://doi.org/10.1002/path.5263
Novak JS, Hogarth MW, Boehler JF, Nearing M, Vila MC, Heredia R, Fiorillo AA, Zhang A, Hathout Y, Hoffman EP, Jaiswal JK, Nagaraju K, Cirak S, Partridge TA. Myoblasts and macrophages are required for therapeutic morpholino antisense oligonucleotide delivery to dystrophic muscle. Nat Commun. 2017 Oct 16;8(1):941. Erratum in: Nat Commun. 2018 Jan 15;9(1):208. Erratum in: Nat Commun. 2018 Mar 23;9(1):1256. PMID: 29038471; PMCID: PMC5643396.
Min YL, Bassel-Duby R, Olson EN. CRISPR Correction of Duchenne Muscular Dystrophy. Annu Rev Med. 2019 Jan 27;70:239-255. Epub 2018 Oct 31. PMID: 30379597; PMCID: PMC6415693.
DOI: https://doi.org/10.1146/annurev-med-081117-010451
Kupatt C, Windisch A, Moretti A, Wolf E, Wurst W, Walter MC. Genome editing for Duchenne muscular dystrophy: a glimpse of the future? Gene Ther. 2021 Sep;28(9):542-548. Epub 2021 Feb 2. PMID: 33531685; PMCID: PMC8455335.
DOI: https://doi.org/10.1038/s41434-021-00222-4
Domenig SA, Bundschuh N, Lenardič A, Ghosh A, Kim I, Qabrati X, D'Hulst G, Bar-Nur O. CRISPR/Cas9 editing of directly reprogrammed myogenic progenitors restores dystrophin expression in a mouse model of muscular dystrophy. Stem Cell Reports. 2022 Feb 8;17(2):321-336. Epub 2022 Jan 6. PMID: 34995499; PMCID: PMC8828535.
DOI: https://doi.org/10.1016/j.stemcr.2021.12.003
Politano L. Read-through approach for stop mutations in Duchenne muscular dystrophy. An update. Acta Myol. 2021 Mar 31;40(1):43-50. PMID: 33870095; PMCID: PMC8033424.
Sun C, Shen L, Zhang Z, Xie X. Therapeutic Strategies for Duchenne Muscular Dystrophy: An Update. Genes (Basel). 2020 Jul 23;11(8):837. PMID: 32717791; PMCID: PMC7463903.
DOI: https://doi.org/10.3390/genes11080837
Seto JT, Ramos JN, Muir L, Chamberlain JS, Odom GL (2012) Gene replacement therapies for duchenne muscular dystro- phy using adeno-associated viral vectors. Curr Gene Ther 12:139-151.
DOI: https://doi.org/10.2174/156652312800840603
Nance ME, Duan D. Perspective on Adeno-Associated Virus Capsid Modification for Duchenne Muscular Dystrophy Gene Therapy. Hum Gene Ther. 2015 Dec;26(12):786-800. Epub 2015 Oct 15. PMID: 26414293; PMCID: PMC4692109.
DOI: https://doi.org/10.1089/hum.2015.107
Zhang Y, Yue Y, Li L, Hakim CH, Zhang K, Thomas GD, Duan D. Dual AAV therapy ameliorates exercise-induced muscle injury and functional ischemia in murine models of Duchenne muscular dystrophy. Hum Mol Genet. 2013 Sep 15;22(18):3720-9. Epub 2013 May 15. PMID: 23681067; PMCID: PMC3749861.
DOI: https://doi.org/10.1093/hmg/ddt224
Loro E, Sengupta K, Bogdanovich S, Whig K, Schultz DC, Huryn DM, Khurana TS. High-throughput identification of post-transcriptional utrophin up-regulators for Duchenne muscle dystrophy (DMD) therapy. Sci Rep. 2020 Feb 7;10(1):2132. Erratum in: Sci Rep. 2020 Feb 28;10(1):4039. PMID: 32034254; PMCID: PMC7005813.
DOI: https://doi.org/10.1038/s41598-020-58737-6
Soblechero-Martín P, López-Martínez A, de la Puente-Ovejero L, Vallejo-Illarramendi A, Arechavala-Gomeza V. Utrophin modulator drugs as potential therapies for Duchenne and Becker muscular dystrophies. Neuropathol Appl Neurobiol. 2021 Oct;47(6):711-723. Epub 2021 Jun 4. PMID: 33999469; PMCID: PMC8518368.
DOI: https://doi.org/10.1111/nan.12735
Vuorinen A, Wilkinson IVL, Chatzopoulou M, Edwards B, Squire SE, Fairclough RJ, Bazan NA, Milner JA, Conole D, Donald JR, Shah N, Willis NJ, Martínez RF, Wilson FX, Wynne GM, Davies SG, Davies KE, Russell AJ. Discovery and mechanism of action studies of 4,6-diphenylpyrimidine-2-carbohydrazides as utrophin modulators for the treatment of Duchenne muscular dystrophy. Eur J Med Chem. 2021 Aug 5;220:113431. Epub 2021 Apr 20. PMID: 33915371.
DOI: https://doi.org/10.1016/j.ejmech.2021.113431
Gehrig SM, van der Poel C, Sayer TA, Schertzer JD, Henstridge DC, Church JE, Lamon S, Russell AP, Davies KE, Febbraio MA, Lynch GS. Hsp72 preserves muscle function and slows progression of severe muscular dystrophy. Nature. 2012 Apr 4;484(7394):394-8. PMID: 22495301.
DOI: https://doi.org/10.1038/nature10980
Thakur SS, Swiderski K, Ryall JG, Lynch GS. Therapeutic potential of heat shock protein induction for muscular dystrophy and other muscle wasting conditions. Philos Trans R Soc Lond B Biol Sci. 2018 Jan 19;373(1738):20160528. PMID: 29203713; PMCID: PMC5717528.
DOI: https://doi.org/10.1098/rstb.2016.0528
Hardee JP, Martins KJB, Miotto PM, Ryall JG, Gehrig SM, Reljic B, Naim T, Chung JD, Trieu J, Swiderski K, Philp AM, Philp A, Watt MJ, Stroud DA, Koopman R, Steinberg GR, Lynch GS. Metabolic remodeling of dystrophic skeletal muscle reveals biological roles for dystrophin and utrophin in adaptation and plasticity. Mol Metab. 2021 Mar;45:101157. Epub 2020 Dec 24. PMID: 33359740; PMCID: PMC7811171.
DOI: https://doi.org/10.1016/j.molmet.2020.101157
Serrano AL, Muñoz-Cánoves P. Fibrosis development in early-onset muscular dystrophies: Mechanisms and translational implications. Semin Cell Dev Biol. 2017 Apr;64:181-190. Epub 2016 Sep 23. PMID: 27670721.
DOI: https://doi.org/10.1016/j.semcdb.2016.09.013
March JT, Golshirazi G, Cernisova V, Carr H, Leong Y, Lu-Nguyen N, Popplewell LJ. Targeting TGFβ Signaling to Address Fibrosis Using Antisense Oligonucleotides. Biomedicines. 2018 Jun 25;6(3):74. PMID: 29941814; PMCID: PMC6164894.
DOI: https://doi.org/10.3390/biomedicines6030074
How to Cite
Dowling, P., Swandulla, D., & Ohlendieck, K. (2023). Cellular pathogenesis of Duchenne muscular dystrophy: progressive myofibre degeneration, chronic inflammation, reactive myofibrosis and satellite cell dysfunction. European Journal of Translational Myology, 33(4). https://doi.org/10.4081/ejtm.2023.11856
Copyright (c) 2023 the Author(s)


This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2023.11856
https://doi.org/10.4081/ejtm.2023.11856