Effects of N-acetylcysteine and metformin treatment on the stereopathological characteristics of uterus and ovary
Accepted: 16 February 2022
HTML: 11
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
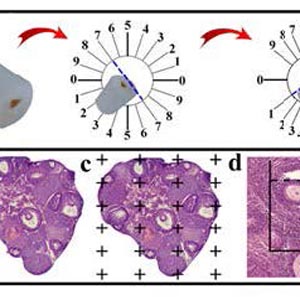
In this study, the stereo-pathological effect of metformin and N-acetyl cysteine is evaluated on the uterus and ovary of polycystic ovary syndrome (PCOS) mice. 96 mature females (8-weekold, weight of 20–30 gr) BALB/c mice were classified into 6 groups including the control group (n= 16), letrozole-induced PCOS group (n=16), PCOS + metformin (n=16), PCOS+NAC (n=16) and a separate control group for NAC (n=16). Another PCOS group was maintained for a month to make sure that features remain till the end of the study. Testosterone level, vaginal cytology and stereological evaluations were assessed. Vaginal cytology in letrozole-receiving mice showed a diestrus phase continuity. Testosterone level, body weight, uterine weight, endometrial volume, myometrial volume, gland volume, stromal volume, epithelial volume, vessel volume, daughter and conglomerate glands, endometrial thickness, and myometrial thickness exhibited an increasing trend in the uterus of PCOS mice. While normal gland and vessel length decreased in the PCOS group. Ovarian volume, corticomedullary volume, primary follicles, secondary follicles, and ovarian cysts were increased in PCOS ovaries. While corpus luteum, primordial, graafian, and atretic follicles showed a decline in the PCOS group. NAC and metformin, however, managed to restore the condition to normal. Given the prevalence of PCOS and its impact on fertility, the use of noninvasive methods is of crucial significance. NAC can control and treat pathological parameters and help as a harmless drug in the treatment of women with PCOS.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2022.10409
https://doi.org/10.4081/ejtm.2022.10409



