Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Comparative study between ureter first approach and conventional open Anderson-Hynes pyeloplasty in paediatric patients: A prospective randomised study
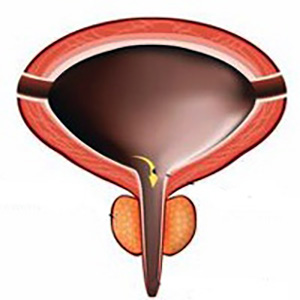
Background: Uretero-pelvic junction obstruction is the most common form of congenital anomaly of the kidney and urinary tract with an incidence of about 1/1.000-1.500 of births and the aetiology and pathogenesis of this anomaly are still unclear until now.
Methods: This is a prospective randomized comparative study conducted from March 2022 to December 2022. Thirty children with uretero-pelvic junction obstruction were included and randomly divided into two groups according to a 1:1 ratio (computer-generated randomization, single blind). Fifteen cases (12 males and 3 female) were subjected to ureter first approach pyeloplasty, and another fifteen (9 males and 6 female) were subjected to conventional Anderson Hynes pyeloplasty.
Results: The mean age of all patients was 6.7 ± 5.4 years in ureter first approach group and 5.1 ± 4.3 years in conventional Anderson-Hynes pyeloplasty group. There were no significant differences between the two groups regarding age, gender, presentation, side, preoperative renogram and post-operative renogram. Also, there were no significant differences between the two groups regarding operative time (in first group 110.3 ± 12.4 and in the second group 111.2 ± 12.0 with p < 0.836), pre and post-operative complication rate. Two cases of urinary tract infections in the first group, one of them having fever, and four cases in the second group, two of them having fever (p < 0.651); four cases of loin pain in the first group and one case in the second group (p < 0.330); one case in the first group having pro- longed leakage of urine for 7 days in post-operative period (p < 0.309). However GFR and t 1⁄2 improved significantly after operation in both groups (p < 0.001).
Conclusions: Ureter first approach is a simple and effective procedure in children with good short term outcomes and could be done safely especially for beginners and less expert surgeons. Finally, it can overcome the problem of long ureteric stricture that may be found intraoperatively because you can shift easily to a flap procedure and complete a tension free anastomosis.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/aiua.2023.11231
https://doi.org/10.4081/aiua.2023.11231